Reem Abdelraouf Elsharkawy1, Sherif I. Elfayoumy MD.2, Ibrahim Abdelbaser MD.1,*, Sherin A. Bakery MD.1
Recibido: 16-07-2022
Aceptado: 23-10-2022
©2023 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 52 Núm. 2 pp. 193-200|https://doi.org/10.25237/revchilanestv5226121150
PDF|ePub|RIS
Abstract
In pediatric cardiac surgery, the use of multimodal analgesia, including a regional analgesic technique reduces opioid consumption and adverse effects. This study aimed to compare the effect of the ultrasound-guided bilateral thoracic erector spinae plane block (ESPB) and paravertebral block (PVB) on postoperative pain score and opioid consumption. This is a single center randomized, controlled, double-blinded, non-inferiority study. A total of 50 eligible pediatric patients, aged 2-10 years, scheduled for elective open cardiac surgery via median sternotomy were recruited. Bilateral ultrasound-guided thoracic ESPB at T4 was performed in patients included in the ESPB group and bilateral PVB was done in patients included in the PVB group by injecting 0.25% bupivacaine 0.4mL/kg on each side. The primary end point was fentanyl consumption during the first 24 h following extubation, while the secondary endpoints were postoperative modified objective pain score (MOPS), time needed to perform the block, intraoperative fentanyl consumption, time to the first analgesic request and the incidence of mechanical complications. Both ESPB and PVB similarly reduced fentanyl consumption during the first 24 h following extubation and MOPS at all time points of measurement. Intraoperative fentanyl consumption and time to first analgesic request were similar in both ESPB and PVB group. The time needed to perform the block was significantly shorter in the ESPB group than the PVB group. Mechanical complications of needle advancement did not occur in any patients. In pediatric patients scheduled for open cardiac surgery via median sternotomy, ultrasound-guided bilateral thoracic ESPB is non-inferior to PVB in providing postoperative analgesia in terms of opioid consumption and pain score. Moreover, ESPB is easier and its performance requires a shorter period than PVB.
Resumen
En cirugía cardíaca pediátrica, el uso de analgesia multimodal, incluida una técnica analgésica regional, reduce el consumo de opioides y los efectos adversos. Este estudio tuvo como objetivo comparar el efecto del bloqueo bilateral del plano del erector de la columna torácica (ESPB) guiado por ecografía y el bloqueo paravertebral (PVB) sobre la puntuación del dolor posoperatorio y el consumo de opiáceos. Este es un estudio de no inferioridad, aleatorizado, controlado, doble ciego, en un solo centro. Se reclutó un total de 50 pacientes pediátricos entre 2 a 10 años, programados para cirugía cardíaca abierta electiva mediante esternotomía media. A los pacientes incluidos en el grupo BES se les realizó EL bloqueo bilateral guiado por ecografía en T4 y a los pacientes incluidos en el grupo BPV se les realizó bilateral mediante la inyección de bupivacaína al 0,25% 0,4 ml/kg en cada lado. El objetivo principal fue el consumo de fentanilo durante las primeras 24 h después de la extubación, mientras que los objetivos secundarios fueron el puntaje de dolor objetivo modificado (MOPS) posoperatorio, el tiempo necesario para realizar el bloqueo, el consumo de fentanilo intraoperatorio, el tiempo hasta la primera solicitud de analgésico y la incidencia de dolor mecánico. Complicaciones
-
Introduction
Pain after cardiac surgery arises mainly from the site of sternotomy incision and to lesser extent from the sites of inserting the drainage tubes. The implementation of perioperative analgesia in pediatric patients undergoing cardiac surgery is challenging because they have unique anatomical characteristics and unpredictable hemodynamic response to pain and opioid analgesics. Traditionally, high-dose IV opioids were used to control pain after cardiac surgery, however this may cause hypotension, bradycardia, respiratory depression, delayed extubation and opioid habituation. In pediatric cardiac surgery, the use of multimodal analgesia, including a regional analgesic technique reduces opioid consumption and their adverse effects[1].
Paravertebral block (PVB) has gained more popularity than other regional analgesic techniques including caudal and epidural for perioperative analgesia in pediatric cardiac surgery[2]. Thoracic paravertebral block provides adequate postoperative analgesia with favorable adverse effects[3],[4]. The use of thoracic PVB in cardiac surgery is associated with decreased pain severity and opioid consumption in both adults[5],[6] and children[2],[7].
Erector spinae plane block (ESPB) is a relatively new facial plane block involving injecting local anesthetics between erector spinae muscle and transverse process[8]. Single shot ESPB provides good postoperative analgesia after many surgeries such as breast surgery[9] and thoracic surgery[10]. In cardiac surgery, few reports have demonstrated the analgesic efficacy of ESPB in both adults[11] and children[12].
The aim of this randomized controlled study was to compare the effect of ultrasound-guided bilateral thoracic ESPB and PVB on postoperative pain score and opioid consumption. Our hypothesis was that, ESPB would be non-inferior to PVB in providing postoperative analgesia in children scheduled for cardiac surgery via median sternotomy.
-
Methods
This single-center prospective, randomized, double-blinded, controlled, non-inferiority study was conducted in our institutional hospital from June 2020 to December 2021 after approval from Mansoura Faculty of Medicine Review Board on May 3, 2020 (IRB code: R.20.04.821). Pan African clinical trial registry approved the registration of this study on May 8, 2020 with unique ID PACTR202005904505939. A total of 50 eligible patients were enrolled. Children aged between 2 and 10 years with American Society of Anesthesiologists physical I & II scheduled for elective open cardiac surgery via median sternotomy were recruited for the study. Informed written consent was signed from the patient legal guardian. Exclusion criteria were history of previous cardiac surgery, urgent surgery, unstable hemodynamics, presence of coagulopathy, neurological dysfunction, mechanically ventilated patient, allergy to study drugs, thoracic spine deformity and history of thoracic vertebrae trauma or surgery. The study was conducted in accordance with the ethical principles of the Declaration of Helsinki with good clinical practice.
-
Randomization and blindness
Patients were randomly allocated to 2 equal groups using computer-generated random numbers before surgery. The patient group assignment was placed in a sealed opaque envelope that was opened at the morning of surgery by an anesthesia resident who was not involved in the study. Data collection was done by experienced nurses who were blind to the patient group allocation. Patients were equally allocated to either the PVB group or the ESPB block group.
-
Management of general anesthesia
The patient received intramuscular midazolam 0.1 mg/ kg, ketamine 3 mg/kg and atropine sulphate 0.015 mg/kg in the preoperative area 15 min before the separation from their guardians. On arrival in the operating room, 5 lead electrocardiography and pulse oximetry were connected to the patient. Anesthesia was induced with intravenous injection of propofol 2 mg/kg, fentanyl 2 pg/kg and rocuronium 0.9 mg/kg to facilitate endotracheal intubation. Arterial and central venous catheters were inserted using the linear high frequency ultrasound transducer under complete sterilization. The patient was also monitored using capnography, urinary catheter and nasopharyngeal temperature probe. Anesthesia was maintained with 1%-2% isoflurane in 50% oxygen/air mixture, fentanyl 1pg/ kg/h and rocuronium 0.3 mg/kg/h with administration of fen- tanyl 3 pg/kg/h increments if heart rate and mean arterial blood pressure rise above 20% from the baseline.
-
Technique of ultrasound-guided ESPB and PVB
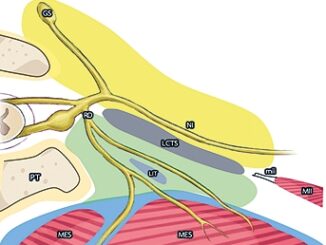
Both ESPB and PVB were performed after the induction of anesthesia in a lateral position. We counted and identified the spinous processes of thoracic vertebrae from cranial to caudal to identify and mark the T4 spinous process. The skin area at the site of needle puncture and around T4 was sterilized with povidone-iodine and 70% isopropyl alcohol, and isolated with sterile drapes. The high-frequency linear transducer of ultrasonography was enclosed within a sterile sheath and placed in a parasagittal position just lateral to T4 spinous process to view the erector spinae muscle, T4 transverse process, superior costotransverse ligament, paravertebral space and pleura (Figure 1). A 50 mm 22-gaug sonographic needle was inserted from cephalad to caudad direction in an in-plane technique aiming at T4 transverse process (ESPB) (Figure 2A) or the paravertebral space between T3 and T4 (PVB) (Figure 2B). In ESPB, the needle tip pierced trapezius, rhomboid major, and erector spinae muscle where the local anesthetic was injected just posterior to the T4 transverse process. In PVB, the needle tip was more deeply advanced between T3 and T4 transverse processes to penetrate the superior costotransverse ligament where the local anesthetic was injected in the paravertebral space just posterior to the pleura. Both ESPB and PVB performed bilaterally by injecting 0.4 mL/kg 0.25% bupivacaine on each side.
-
Intraoperative management
Standard median sternotomy incision was used for all surgeries. The patient received heparin 300-400 i.u/kg via the central venous catheter to increase the activated clotting time above 480 sec before instituting cardiopulmonary bypass. The pump flow was (100-150) mL/kg/min and patient temperature was maintained at (33-35) °C. After completion of the surgical repair of the cardiac anomaly and fulfilling the criteria of weaning from cardiopulmonary bypass (CPB), patient was separated from the bypass. At the end of surgery, the patient was transferred to the intensive care unit (ICU).
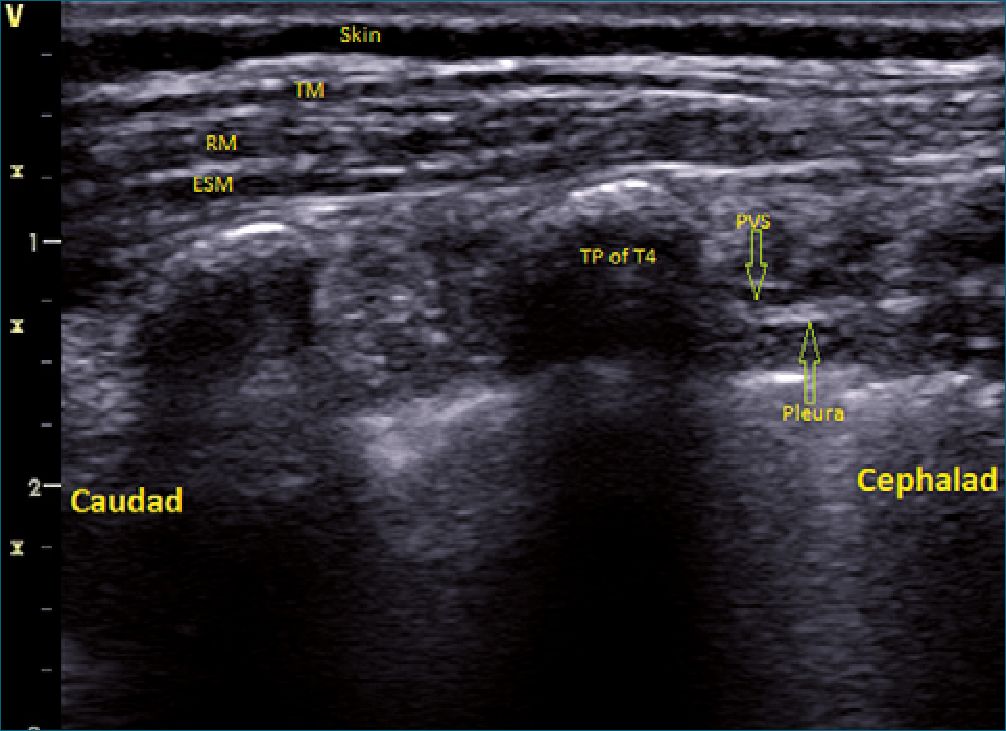
Figure 1. Ultrasound image showing trapezius muscle (TM), rhomboid muscle (RM), erector spinae muscle (ESM), transverse process (TP) of T4, superior costotransverse ligament, the paravertebral space (PVS) and pleura.
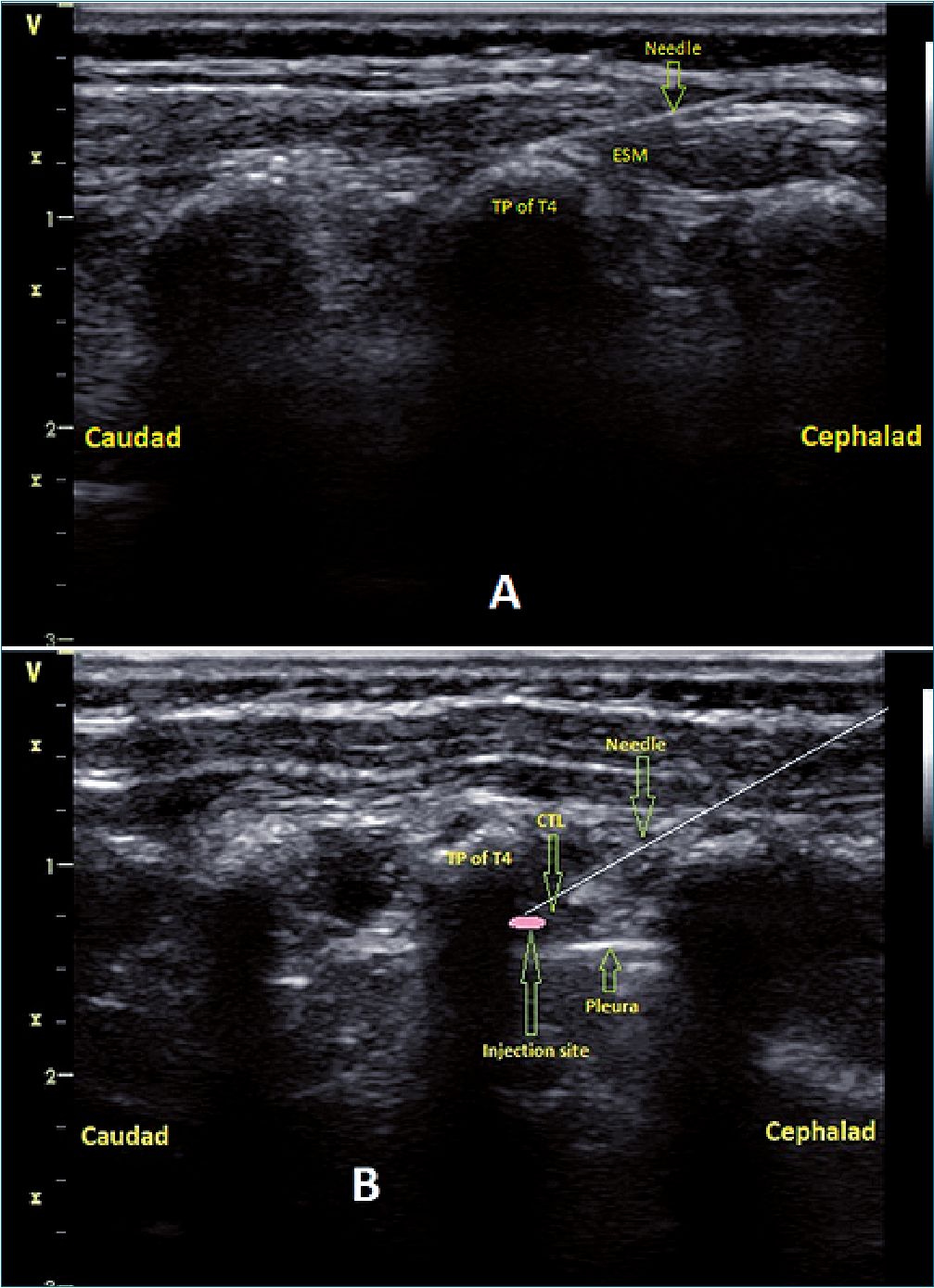
Figure 2. Ultrasound image showing the targeted position of needle tip to inject the local anesthetic in erector spinae plane block (2A) and paravertebral block; (2B). TP: transverse process; CTL: costotransverse ligament.
-
Postoperative management
In the ICU patient was monitored using the same intra- operative monitoring parameters. The patient was extubated within few hours once the criteria of extubation were fulfilled (adequate level of consciousness, good breathing parameters, hemodynamic stability on minimal or no inotropic, acceptable arterial blood gases and the absence of significant bleeding). The patients received intravenous paracetamol 15 mg/kg/8h.
Postoperative pain was assessed using 10 points Modified Objective Pain Score (MOPS).[13]
Fentanyl was given as a rescue analgesic at a dose of 1pg/ kg if MOPS was > 3 at rest.
-
Data collection
The primary end point was fentanyl consumption during the first 24 h following extubation. The secondary endpoints were MOPS measured at 0, 1, 2, 6, 12, 18, and 24 h after extubation, time needed to perform the block (defined as time be- tween placing the linear transducer on skin till the end of local anesthetic injection and withdrawal of the block needle), intraoperative fentanyl consumption, time to the first analgesic request that measured after extubation, time to extubation and the duration of ICU stay. The incidence of traumatic complications related to the block needle insertion (pneumothorax, vascular injury and neurological injury), local anesthetic toxicity and postoperative complications such as pruritus and vomiting were all reported.
-
Sample size and statistical analyses
The sample size was calculated using PASS 15 software using the non-inferiority test for the difference between 2 means. The primary outcome was the total fentanyl consumption (pg/ kg) during the first postoperative 24 h following extubation. As there were no previous similar studies, we used the results of our preliminary study (unpublished) that included 5 patients in each group to calculate the needed sample size, in which the mean ± SD 24 h fentanyl consumption (pg/kg) was 5.2 ± 1.4 with PVB and 5.9 ± 2.6 with ESPB. The calculated sample size using one-sided, two-sample t-test was 20 patients per group achieved 80% power. The margin of non-inferiority was assumed to be 1, the difference between the 2 means was 0.7 and, standard deviations were 2.6 and 1.4. The significance level (alpha) of the test is 0.05. The number of patients in increased to 25 per group to avoid the probable dropouts.
The statistical data analysis was done using IBM SPSS Version 21.0. Armonk, NY: IBM Corp. Kolmogorov-Smirnov test was used to check the normality of quantitative data distribution. Data analysis was done by the comparison between ESPB and PVB group. Normally distributed quantitative data are ex- pressed as mean ± standard deviation (SD) and were analyzed by unpaired student t-test. Categorical data are presented as number (proportion) and was tested with Chi-square test. Non-parametric data are presented as median (IQR. Q1, Q3) and were analyzed using Mann-Whitney U test. P < 0.05 at confidence interval 95% is statistically significant.
The non-inferiority of ESPB to PVB was confirmed because the non-inferiority margin (1) is greater than the upper limit of 95% confidence interval (0.804) of the primary outcome (24 h postoperative fentanyl consumption).
-
Results
Of 50 patients who were recruited, 6 were excluded, 4 were not meeting the inclusion criteria and the legal guardians of other 2 declined to participate (Figure 3). The remaining 44 patients were randomly allocated to the ESPB group (n=22) and PVB group (n = 22), all of them completed the study and under- went the final analysis (Figure 3).
No significant differences were observed in patient characteristics (age, gender, weight, height and body surface area) and surgical characteristics (CPB time, aortic clamping time, du- ration of surgery and type of surgery) between the patients in the ESPB group and PVB group (Table 1).
As regard the primary outcome, there was no significant difference (p = 0.612) in the mean ± SD fentanyl consumption (pg/kg) during the first postoperative 24 h after extubation between the ESPB group (4.9 ± 1.7) and PVB group (4.6 ± 1.7) (Table 2).
The median MOPS at rest was similar in both study groups all over the first postoperative 24 h and was kept < 3 except at 18h (Figure 4). The median (IQR) intraoperative fentanyl consumption (pg/kg) was similar (p = 0.083) in both ESPB and PVB group (9[8]-[10], 8[7]-[9] respectively) (Table 2). The median (IQR) time to first analgesic request (h) was similar (p = 0.721) in both ESPB and PVB group (8[6]-[8], 7.5[6]-[10] respectively) (Table 2). There were no significant differences in the median (IQR) time to extubation (h) and the mean ± SD ICU stay (h) on comparing ESPB group with the PVB group (2 [2]-[3] & 21.8 ± 2.6 vs 1[2]-[3] & 21.6 ± 3.6, respectively) (Table 2).
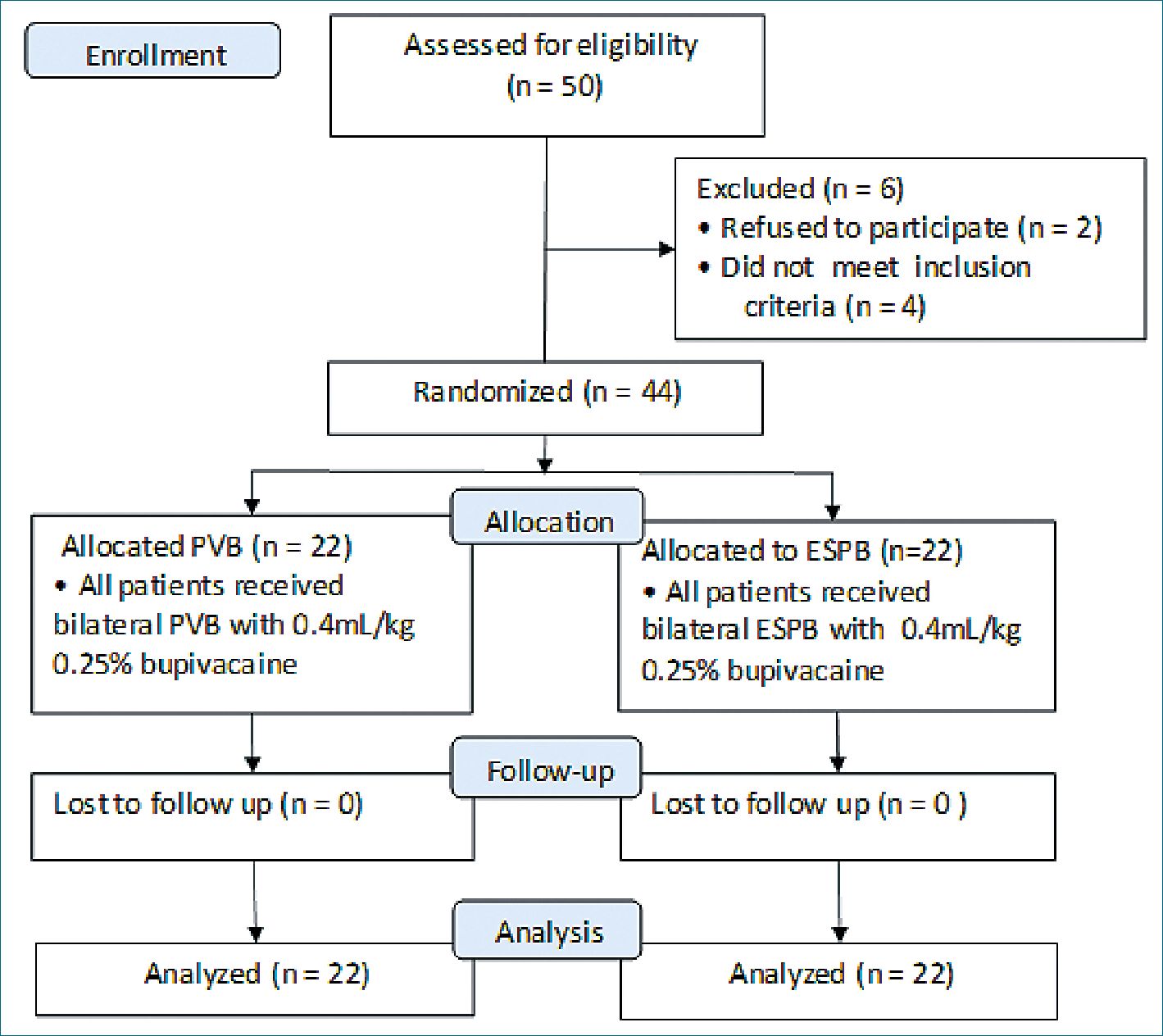
Figure 3. Study flowchart. PVB: paravertebral block; ESPB: erector spinae plane block.
Table 1. Patients and surgical characteristics
| Variable | ESPB group (n = 22) | PVB group (n = 22) | P value |
| Age (year) | 5.45 [3.8-7] | 4.7 [3.8-6.5] | 0.897 |
| Gender (M/F) | 9/13 | 11/11 | 0763 |
| Height (cm) | 108 ± 13.8 | 106 ± 14.5 | 0.745 |
| Weight (kg) | 13.25 [12-17] | 13.5 [12-16] | 0.750 |
| BSA (m2) | 0.66 ± 0.09 | 0.61 ± 0.11 | 0.193 |
| Aortic clamping time (min) | 35.5 [25-43] | 33 [26-40] | 0.565 |
| CPB time (min) | 60.2 ± 15.1 | 59.7 ± 10.7 | 0.891 |
| Duration of surgery (min) | 194 ± 20 | 197 ±16 | 0.701 |
| Type of surgical repair: VSD | 10 | 13 | |
| ASD | 10 | 7 | 0.631 |
| AVSD | 2 | 2 |
Non-parametric continuous variables are presented as median (IQR. Q1, Q3), parametric continuous variables are presented as mean ±SD and categorial variables are presented as number. ESPB: erector spinae plane block; PVB: paravertebral block; BSA: body surface area; CPB: cardiopulmonary bypass; ASD: atrial septal defect, VSD: ventricular septal defect; AVSD: atrioventricular septal defect.
| Table 2. Intraoperative fentanyl consumption, postoperative variables, characteristics of the block and postoperative | ||||
| complications | ||||
| Variable | ESPB group (n = 22) | PVB group (n = 22) | P value | 95% CI |
| Intraoperative fentanyl (p/kg) consumption | 9 [8-10] | 8 [7-9] | 0.083 | |
| 24h postoperative fentanyl (p/kg) consumption | 4.9 ± 1.7 | 4.6 ± 1.7 | 0.612 | -1.350, 0.804 |
| Time to first analgesic request (h) | 8 [6-8] | 7.5 [6-10] | 0.721 | |
| Time to extubation (h) | 2 [2-3] | 1 [2-3] | 0.359 | |
| Duration of ICU stay (h) | 21.8 ± 2.6 | 21.6 ± 3.6 | 0.817 | -2.197, 1.742 |
| Time needed to perform the bilateral block (min) | 7.5 [7-9] | 12 [10-13] | < 0.001* | |
| Complications of the block | 0 | 0 | ||
| Postoperative;
Vomiting |
5 | 5 | 1.000 | |
| Pruritus | 4 | 5 | 1.000 | |
Non-parametric continuous variables are presented as median (IQR. Q1, Q3), parametric continuous variables are presented as mean ±SD and categorical variables are presented as number. ESPB: erector spinae plane block; PVB: paravertebral block; CI: confidence interval; ICU: intensive care unit. P<0.05 is statistically significant.
The median (IQR) time (min) needed to perform bilateral block was significantly shorter (p< 0.001) in the ESPB group (7.5[7]-[9]) than thePVB group (12[10]-[13]) (Table 2). We didn’t observe any mechanical complications related to needle advancement (pneumothorax or vascular injury) or local anesthetic toxicity. The number of patients who developed postoperative vomiting and pruritus was similar in both ESPB group and PVB group (5, 4 & 5, 5 respectively) (Table 2).
-
Discussion
This randomized, controlled, double blind study demonstrated the non-inferiority of bilateral thoracic ESPB compared to PVB in reducing post-extubation 24 h opioid consumption in pediatric patients who underwent open cardiac surgery as the non-inferiority margin was higher than the upper limit of 95% confidence interval of the primary outcome. There were no significant differences between ESPB and PVB regarding intraoperative fentanyl consumption, postoperative MOPS, time to first analgesic request, time to extubation, the incidence of postoperative complications and ICU length of stay. Further-more, performing ESPB needed shorter time than PVB.
The current study showed the non-inferiority of single shot ESPB to PVB in providing postoperative analgesia after cardiac surgery. Paravertebral block has been shown to provide effective analgesia in terms of opioid consumption and pain scores after cardiac surgery[2],[5]-[7] To the best of our knowledge, this is the first randomized clinical trial that compared the effects of ESPB and PVB on postoperative analgesia after cardiac surgery. Kaushal B, et al. performed bilateral thoracic ESPB in 40 pediatric patients who underwent cardiac surgery via median sternotomy and compared its postoperative analgesic effects with those of patients with no block, they found that ESPB was associated with superior and effective postoperative analgesia compared with the control[12]. Macaire P et al., included 50 pediatric patients who were scheduled for cardiac surgery using midline sternotomy in their study that compared the postoperative opioid consumption in patients who received bilateral ESPB with patients who received placebo.[14] Macaire and colleagues found that the use of ESPB in pediatric cardiac surgery provided superior and a more effective postoperative analgesia in terms of morphine consumption and pain scores than the control. In adults open cardiac surgery, several studies have been demonstrated the efficacy of ESPB in reducing post- operative pain severity and opioids requirements[11],[15]-[17].
The results of our study are consistent with the results of previous studies involving non-cardiac surgeries. The non-inferiority of ESPB to PVB in reducing postoperative opioid requirements and pain has been shown after video-assisted thoracic surgery[18],[19] and breast surgery[20]. After thoracotomy, the analgesia provided by single injection ESPB is comparable to PVB[21].
In this study we injected single-dose of 0.25% bupivacaine 0.4 mL/kg bilaterally at the level of transverse process of the fourth thoracic vertebra for ESPB or in the paravertebral space between the third and fourth thoracic vertebra. In our study the median time to first analgesic request was similar in both groups, 8 h in ESPB and 7.5 h in PVB indicating the short duration of postoperative analgesia of single injection of both ESPB and PVB.
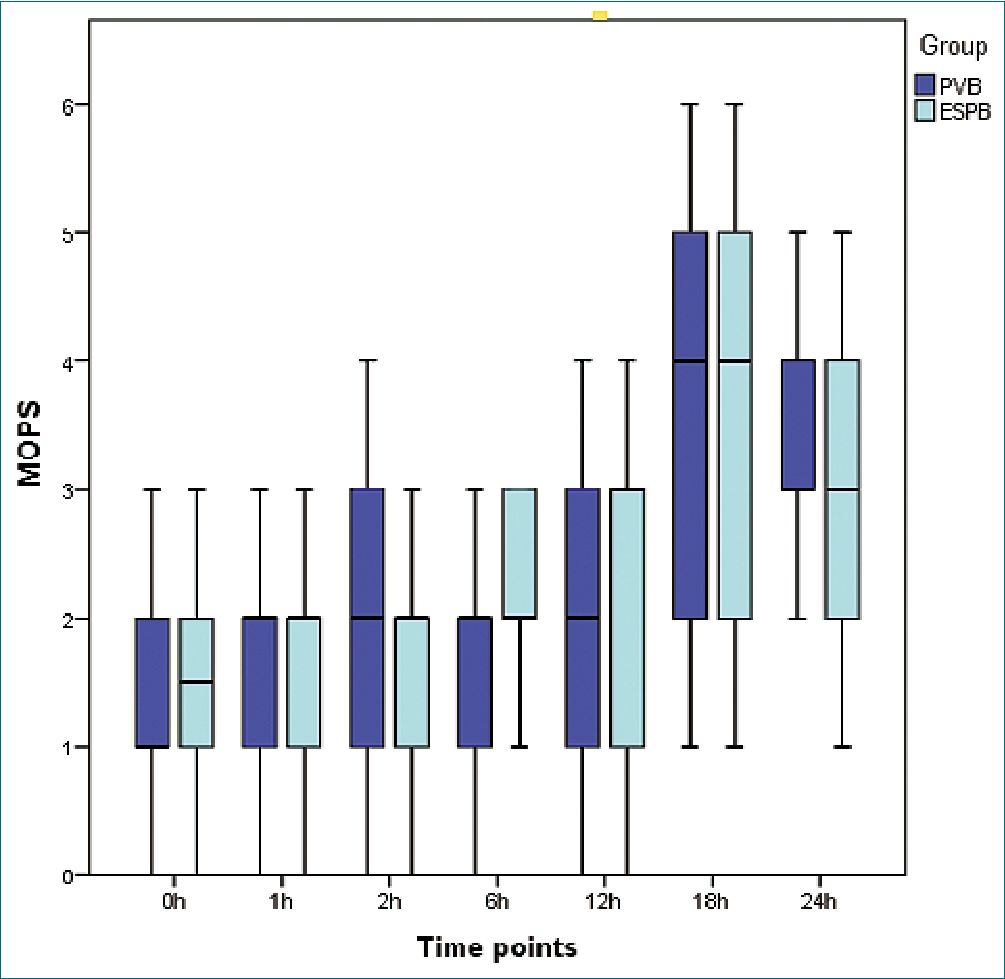
Figure 4. Modified Objective Pain Score (MOPS) measured at 0 h, 1 h, 2 h, 6 h, 12 h, 18 h and 24 h after extubation. PVB: paravertebral block; ESPB: erector spinae plane block.
Thoracic PVB has been shown to provide equivalent analgesia to thoracic epidural block with lower incidence of adverse effects such as hypotension, bradycardia and urine retention[22]. Therefore, thoracic PVB may be used as an alternative to epidural analgesia, however, the paravertebral space is small with probable risk of pleural puncture even with ultrasound guidance especially with less skilled anesthesiologists. Erector spinae plane block gives analgesia similar to PVB and is a relatively superficial block with transverse process acting as a barrier against pleural puncture by the needle tip. The mechanism of action of ESPB is still not fully understood and several mechanisms have been postulated. Ivanusic et al. in their cadaveric study reported the craniocaudal, posterior and lateral spread of local anesthetic to block the dorsal rami[23]. Adhikary et al., found that the local anesthetic spread between the transverse process and erector spinae muscle with extensive spread to the more anterior structures including the paravertebral and epidural spaces[24]. One possible mechanism is the paravertebral spread of local anesthetics from its site of injection between transverse process and erector spinae muscle 4 segments cranially and 3 segments caudally[25]. Epidural spread of the local anesthetics is also a potential mechanism of action as several studies reported bilateral sensory blockade in some patients after unilateral ESPB that was attributed to the epidural spread[26]-[28].
In this study all patients in both groups were extubated early (less than 6 h) and they were shortly stayed in ICU. We performed ESPB and PVB before surgery and this reduced the total intraoperative opioid consumption. For postoperative analgesia, we used a multimodal analgesic technique consisting of a regional block, intravenous paracetamol and opioid, all of these could act synergistically and reduced postoperative opioid consumption. Multimodal analgesia is widely used to control pain after pediatric cardiac surgery[29]. Reduction of perioperative opioids consumption minimizes their adverse effects and allows early extubation.
We found that the time needed to perform ESPB was shorter than PVB indicating the ease of doing ESPB that can be done by a non-highly skilled anesthesiologist. This is in agreement with previous studies that compared ESPB with PVB[30],[31]. This can be explained by some reasons. First, the anatomical landmarks of ESPB (transverse process and erector spinae muscle) are more superficial and obvious with ultrasonography in comparison with the small deep paravertebral space. Second, needle advancement to the paravertebral space for PVB re- quires inserting the needle in more acute angle and for longer distance compared to ESPB resulting in better needle visualization in the later.
We didn’t report the incidence of any mechanical complications or local anesthetic toxicity in ESPB and PVB indicating their safety. The incidence of postoperative vomiting and pruritus was similar in both groups and was related to opioid analgesics. This study has some limitations. First, we used single-dose injection of 0.25% bupivacaine that produced postoperative analgesia of short duration. Insertion of catheters for local anesthetic infusion to obtain prolonged ESPB and PVB postoperative analgesia is recommended, but the pediatric size of epidural catheter was unavailable in our institutional hospital. Second, the small sample size of this study did not allow us to comment more accurately on the safety of both ESPB and PVB. Third, we could not test the dermatomal sensory spread of both ESPB and PVB as the block was performed after induction of anesthesia. Fourth, we did not measure the serum local anesthetic levels because the laboratories in our hospital did not have this technology.
-
Conclusion
In pediatric patients scheduled for open cardiac surgery via median sternotomy, ultrasound-guided bilateral thoracic ESPB is non-inferior to PVB in providing postoperative analgesia in terms of opioid consumption and pain score. Moreover, ESPB is easier and its performance requires shorter period than PVB.
Conflict of interest: There is no conflict of interest to declare.
Funding: No funding was received.
IRB number: The Institutional Research Board, Faculty of Medicine, Mansoura University approved the study protocol on May 3, 2020 (IRB code: R.20.04.821).
Clinical trial registration number: The study protocol was registered at Pan African Clinical Trial Registry with unique ID (PAC- TR202005904505939).
References
1. Monahan A, Guay J, Hajduk J, Suresh S. Regional Analgesia Added to General Anesthesia Compared With General Anesthesia Plus Systemic Analgesia for Cardiac Surgery in Children: A Systematic Review and Meta-analysis of Randomized Clinical Trials. Anesth Analg. 2019 Jan;128(1):130–6. https://doi.org/10.1213/ANE.0000000000003831 PMID:30300178
2. Sahajanandan R, Varsha AV, Kumar DS, Kuppusamy B, Karuppiah S, Shukla V, et al. Efficacy of paravertebral block in “Fast-tracking” pediatric cardiac surgery – Experiences from a tertiary care center. Ann Card Anaesth. 2021;24(1):24–9. https://doi.org/10.4103/aca.ACA_83_19 PMID:33938827
3. Richardson J, Lönnqvist PA. Thoracic paravertebral block. Br J Anaesth. 1998 Aug;81(2):230–8. https://doi.org/10.1093/bja/81.2.230 PMID:9813528
4. Tighe SQ. Paravertebral block. Anaesthesia. 2002 May;57(5):511–2. https://doi.org/10.1046/j.1365-2044.2002.262618.x PMID:11966569
5. Sun L, Li Q, Wang Q, Ma F, Han W, Wang M. Bilateral thoracic paravertebral block combined with general anesthesia vs. general anesthesia for patients undergoing off-pump coronary artery bypass grafting: a feasibility study. BMC Anesthesiol. 2019 Jun;19(1):101. https://doi.org/10.1186/s12871-019-0768-9 PMID:31185919
6. El Shora HA, El Beleehy AA, Abdelwahab AA, Ali GA, Omran TE, Hassan EA, et al. Bilateral Paravertebral Block versus Thoracic Epidural Analgesia for Pain Control Post-Cardiac Surgery: A Randomized Controlled Trial. Thorac Cardiovasc Surg. 2020 Aug;68(5):410–6. https://doi.org/10.1055/s-0038-1668496 PMID:30114712
7. El Bendary HM, Abd El Baser II. Bilateral single bupivacaine injection ultrasound-guided paravertebral block facilitates early extubation and reduces perioperative opioids requirements in on-pump pediatric cardiac surgery. Ain-Shams J Anaesthesiol. 2015;8(3):287–93. https://doi.org/10.4103/1687-7934.159001.
8. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: A Novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621–7. https://doi.org/10.1097/AAP.0000000000000451 PMID:27501016
9. Ohgoshi Y, Ikeda T, Kurahashi K. Continuous erector spinae plane block provides effective perioperative analgesia for breast reconstruction using tissue expanders: A report of two cases. J Clin Anesth. 2018 Feb;44:1–2. https://doi.org/10.1016/j.jclinane.2017.10.007 PMID:29065334
10. Pirsaharkhiz N, Comolli K, Fujiwara W, Stasiewicz S, Boyer JM, Begin EV, et al. Utility of erector spinae plane block in thoracic surgery. J Cardiothorac Surg. 2020 May;15(1):91. https://doi.org/10.1186/s13019-020-01118-x PMID:32398105
11. Krishna SN, Chauhan S, Bhoi D, Kaushal B, Hasija S, Sangdup T, et al. Bilateral Erector Spinae Plane Block for Acute Post-Surgical Pain in Adult Cardiac Surgical Patients: A Randomized Controlled Trial. J Cardiothorac Vasc Anesth. 2019 Feb;33(2):368–75. https://doi.org/10.1053/j.jvca.2018.05.050 PMID:30055991
12. Kaushal B, Chauhan S, Magoon R, Krishna NS, Saini K, Bhoi D, et al. Efficacy of Bilateral Erector Spinae Plane Block in Management of Acute Postoperative Surgical Pain After Pediatric Cardiac Surgeries Through a Midline Sternotomy. J Cardiothorac Vasc Anesth. 2020 Apr;34(4):981–6. https://doi.org/10.1053/j.jvca.2019.08.009 PMID:31515190
13. Wilson GA, Doyle E. Validation of three paediatric pain scores for use by parents. Anaesthesia. 1996 Nov;51(11):1005–7. https://doi.org/10.1111/j.1365-2044.1996.tb14991.x PMID:8943588
14. Macaire P, Ho N, Nguyen T, Nguyen B, Vu V, Quach C, et al. Ultrasound-Guided continuous thoracic erector spinae plane block within an enhanced recovery program is associated with decreased opioid consumption and improved patient postoperative rehabilitation after open cardiac surgery-a patient-matched, controlled before-and-after study. J Cardiothorac Vasc Anesth. 2019 Jun;33(6):1659–67. https://doi.org/10.1053/j.jvca.2018.11.021 PMID:30665850
15. Nagaraja PS, Ragavendran S, Singh NG, Asai O, Bhavya G, Manjunath N, et al. Comparison of continuous thoracic epidural analgesia with bilateral erector spinae plane block for perioperative pain management in cardiac surgery. Ann Card Anaesth. 2018;21(3):323–7. https://doi.org/10.4103/aca.ACA_16_18 PMID:30052229
16. Gawęda B, Borys M, Belina B, Bąk J, Czuczwar M, Wołoszczuk-Gębicka B, et al. Postoperative pain treatment with erector spinae plane block and pectoralis nerve blocks in patients undergoing mitral/tricuspid valve repair – a randomized controlled trial. BMC Anesthesiol. 2020 Feb;20(1):51. https://doi.org/10.1186/s12871-020-00961-8 PMID:32106812
17. Wasfy S, Kamhawy G, Omar A, Abd El Aziz H. Bilateral continuous erector spinae block versus multimodal intravenous analgesia in coronary bypass surgery. A Randomized Trial. Egypt J Anaesth. 2021;37(1):152–8. https://doi.org/10.1080/11101849.2021.1904548.
18. Taketa Y, Irisawa Y, Fujitani T. Comparison of ultrasound-guided erector spinae plane block and thoracic paravertebral block for postoperative analgesia after video-assisted thoracic surgery: a randomized controlled non-inferiority clinical trial. Reg Anesth Pain Med. 2019 Nov;•••:rapm-2019-100827. https://doi.org/10.1136/rapm-2019-100827 PMID:31704789
19. Zhao H, Xin L, Feng Y. The effect of preoperative erector spinae plane vs. paravertebral blocks on patient-controlled oxycodone consumption after video-assisted thoracic surgery: A prospective randomized, blinded, non-inferiority study. J Clin Anesth. 2020 Jun;62:109737. https://doi.org/10.1016/j.jclinane.2020.109737 PMID:32092617
20. Aoyama Y, Sakura S, Tsuchiya R, Wittayapairoj A, Saito Y. Erector Spinae Plane Block and Paravertebral Block for Breast Surgery: A Retrospective Propensity-Matched Noninferiority Trial. J Pain Res. 2020 Sep;13:2367–76. https://doi.org/10.2147/JPR.S265015 PMID:33061552
21. Fang B, Wang Z, Huang X. Ultrasound-guided preoperative single-dose erector spinae plane block provides comparable analgesia to thoracic paravertebral block following thoracotomy: a single center randomized controlled double-blind study. Ann Transl Med. 2019 Apr;7(8):174. https://doi.org/10.21037/atm.2019.03.53 PMID:31168455
22. Joshi GP, Bonnet F, Shah R, Wilkinson RC, Camu F, Fischer B, et al. A systematic review of randomized trials evaluating regional techniques for postthoracotomy analgesia. Anesth Analg. 2008 Sep;107(3):1026–40. https://doi.org/10.1213/01.ane.0000333274.63501.ff PMID:18713924
23. Ivanusic J, Konishi Y, Barrington MJ. A Cadaveric Study Investigating the Mechanism of Action of Erector Spinae Blockade. Reg Anesth Pain Med. 2018 Aug;43(6):567–71. https://doi.org/10.1097/AAP.0000000000000789 PMID:29746445
24. Adhikary SD, Bernard S, Lopez H, Chin KJ. Erector Spinae Plane Block Versus Retrolaminar Block: A Magnetic Resonance Imaging and Anatomical Study. Reg Anesth Pain Med. 2018 Oct;43(7):756–62. https://doi.org/10.1097/AAP.0000000000000798 PMID:29794943
25. Chin KJ, Adhikary S, Sarwani N, Forero M. The analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017 Apr;72(4):452–60. https://doi.org/10.1111/anae.13814 PMID:28188621
26. Schwartzmann A, Peng P, Maciel MA, Forero M. Mechanism of the erector spinae plane block: insights from a magnetic resonance imaging study. Can J Anaesth. 2018 Oct;65(10):1165–6. https://doi.org/10.1007/s12630-018-1187-y PMID:30076575
27. Tulgar S, Selvi O, Ahiskalioglu A, Ozer Z. Can unilateral erector spinae plane block result in bilateral sensory blockade? Can J Anaesth. 2019 Aug;66(8):1001–2. https://doi.org/10.1007/s12630-019-01402-y PMID:31114943
28. Altıparmak B, Korkmaz Toker M, Uysal AI. Potential mechanism for bilateral sensory effects after unilateral erector spinae plane blockade in patients undergoing laparoscopic cholecystectomy. Can J Anaesth. 2020 Jan;67(1):161–2. https://doi.org/10.1007/s12630-019-01436-2 PMID:31240612
29. Horvath R, Halbrooks EF, Overman DM, Friedrichsdorf SJ. Efficacy and Safety of Postoperative Dexmedetomidine Administration in Infants and Children Undergoing Cardiac Surgery: A Retrospective Cohort Study. J Pediatr Intensive Care. 2015 Sep;4(3):138–45. https://doi.org/10.1055/s-0035-1559820 PMID:31110863
30. Swisher MW, Wallace AM, Sztain JF, Said ET, Khatibi B, Abanobi M, et al. Erector spinae plane versus paravertebral nerve blocks for postoperative analgesia after breast surgery: a randomized clinical trial. Reg Anesth Pain Med. 2020 Apr;45(4):260–6. https://doi.org/10.1136/rapm-2019-101013 PMID:31969443
31. Moustafa MA, Alabd AS, Ahmed AM, Deghidy EA. Erector spinae versus paravertebral plane blocks in modified radical mastectomy: randomised comparative study of the technique success rate among novice anaesthesiologists. Indian J Anaesth. 2020 Jan;64(1):49–54. https://doi.org/10.4103/ija.IJA_536_19 PMID:32001909

 ORCID
ORCID