Andrés Sebastián Viteri Hinojosa1,* Galo Sebastián Avalos Vega1, María Paula García Cevallos1, Luis Felipe Rivera Mora2
Recibido: 13-04-2024
Aceptado: 04-06-2024
©2025 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 54 Núm. 1 pp. 3-10|https://doi.org/10.25237/revchilanestv54n1-01
PDF|ePub|RIS
Abstract
Ambulatory surgery is on the rise due to its lower costs and quicker recovery, making the choice between general anesthesia (GA) and regional anesthesia (RA) crucial in traumatic procedures. A thorough search of studies published between 2010 and 2024 in PubMed, MEDLINE, Embase, and Google Scholar yielded twelve studies comparing both modalities. Benefits of RA include fewer postoperative pain episodes, shorter hospital stays, and, in some cases, a decreased need for opioids, particularly following ankle and wrist surgeries. However, the complexity of surgery and patient characteristics influence outcomes. While some studies clearly highlight the advantages of RA, others find similar outcomes between GA and RA. Optimizing patient outcomes requires personalized anesthesia strategies, emphasizing the need for further research to determine the best option for different types of ambulatory operations.
Resumen
La cirugía ambulatoria está en aumento debido a sus costos más bajos y a una recuperación más rápida, lo que hace que la elección entre la anestesia general (GA) y la anestesia regional (RA) sea crucial en procedimientos traumáticos. Una exhaustiva búsqueda de estudios publicados entre 2010 y 2024 en PubMed, MEDLINE, Embase y Google Scholar, arrojó doce estudios comparando ambas modalidades. Los beneficios de la RA incluyen menos episodios de dolor posoperatorio, estancias hospitalarias más cortas y, en algunos casos, una disminución en la necesidad de opioides, particularmente después de cirugías de tobillo y muñeca. Sin embargo, la complejidad de la cirugía y las características del paciente influyen en los resultados. Mientras que algunos estudios resaltan claramente las ventajas de la RA, otros encuentran resultados similares entre GA y RA. Optimizar los resultados del paciente requiere estrategias de anestesia personalizadas, enfatizando la necesidad de más investigaciones para determinar la mejor opción para diferentes tipos de operaciones ambulatorias.
-
Introduction
Recent years have seen a rise in the use of ambulatory surgery, also referred to as outpatient or day surgery, because of its possible advantages, which include lower costs, shorter hospital stays, and speedier patient recovery[1]. Common instances handled in ambulatory settings include
trauma injuries like fractures that need surgical intervention. The choice of anesthesia in these situations is critical to the treatment and results of the patient. In traumatic procedures, two primary forms of anesthesia are used: general anesthesia (GA) and regional anesthesia (RA). While RA involves numbing a particular part of the body, enabling patients to stay awake and maybe endure fewer systemic adverse effects, GA offers total unconsciousness and pain management during the treatment[2]. The difficulty of the procedure, the patient’s medical condition, the surgeon’s choice, and other criteria are often taken into consideration while choosing an anesthesia type. There is ongoing discussion over the relative efficacy and safety results of GA and RA, despite their common use in ambulatory traumatic procedures. While some research suggests that RA is more likely than GA to result in a quicker recovery, less pain after surgery, and fewer systemic problems, other studies contend that GA may be more appropriate for operations since it offers better intraoperative circumstances and pain management[3],[4].
Many systematic reviews are present on the comparison of general versus regional anesthesia in different fracture surgeries. For example, A meta-analysis was carried out by Roh et al., to assess the relative merits of regional anesthesia and general anesthesia in the postoperative treatment of pain after distal radius fracture surgery[3]. Comparing regional anesthesia to general anesthesia, the findings showed a substantial reduction in postoperative pain ratings after two hours (SMD -2.03; 95% CI -2.88 to -1.17). After 12 hours after surgery, there were no significant variations in pain ratings between the two anesthetic kinds, nevertheless. According to the results, there is a noticeable rise in opioid consumption on the first day after discharge, which may be related to rebound pain, even if regional anesthesia may provide analgesic superiority in the early postoperative period and reduce total opioid usage. To examine the effects of regional anesthesia (RA) with general anesthesia (GA) on postoperative complications in patients having lower extremity amputation (LEA), Mufarrih et al., carried out another systematic review and meta-analysis[5]. In comparison to RA, GA was linked to a greater risk of sepsis and respiratory failure, according to the meta-analyses. But there is no systematic review on ambulatory traumatic surgeries. Therefore, the objective of this systematic study is to evaluate the effects of regional anesthesia (RA) vs general anesthesia (GA) in ambulatory traumatic procedures. Our goal is to assess the effectiveness, safety, recovery times, and financial effects of different anesthetic methods by examining current research on a range of orthopedic operations, such as spine surgery, total joint arthroplasty, and knee arthroscopy. Our goal is to give evidence-based insights to improve patient outcomes and clinician decision-making in ambulatory traumatic procedures by a thorough synthesis of the literature. To compare the effectiveness of GA against RA in ambulatory traumatic procedures, this systematic review will critically analyse and assess the material that is currently accessible.
-
Methodology
-
Search strategy
A systematic search of electronic databases, including PubMed, MEDLINE, Embase, and Google Scholar, is being conducted to identify relevant studies published between 2010 and 2024. The search strategy utilizes combinations of keywords related to “general anesthesia,” “regional anesthesia,” “ambulatory surgery,” “traumatic injuries”, “fractures”, and outcomes. Boolean operators (AND, OR) are used to combine these terms effectively (Figure 1).
-
Study selection
Two independent reviewers screened the titles and abstracts of identified articles to assess their eligibility for inclusion. Fulltext articles meeting the predefined criteria are retrieved for further evaluation.
-
Inclusion criteria
• Studies that compare outcomes of general anesthesia versus regional anesthesia in ambulatory traumatic surgeries.
• Randomized controlled trials, prospective cohort studies, and retrospective cohort studies are included.
• Only studies published in English are considered.
-
Exclusion criteria
• Studies not directly comparing general anesthesia with regional anesthesia.
• Case reports, editorials, reviews, and conference abstracts are excluded.
• Studies published in languages other than English are excluded.
-
Data extraction
Relevant data are being extracted from the selected studies, including study characteristics (author, year, study design), type of anesthesia, surgical procedures, and outcomes assessed (e.g., pain, recovery time, complications).
-
Quality assessment
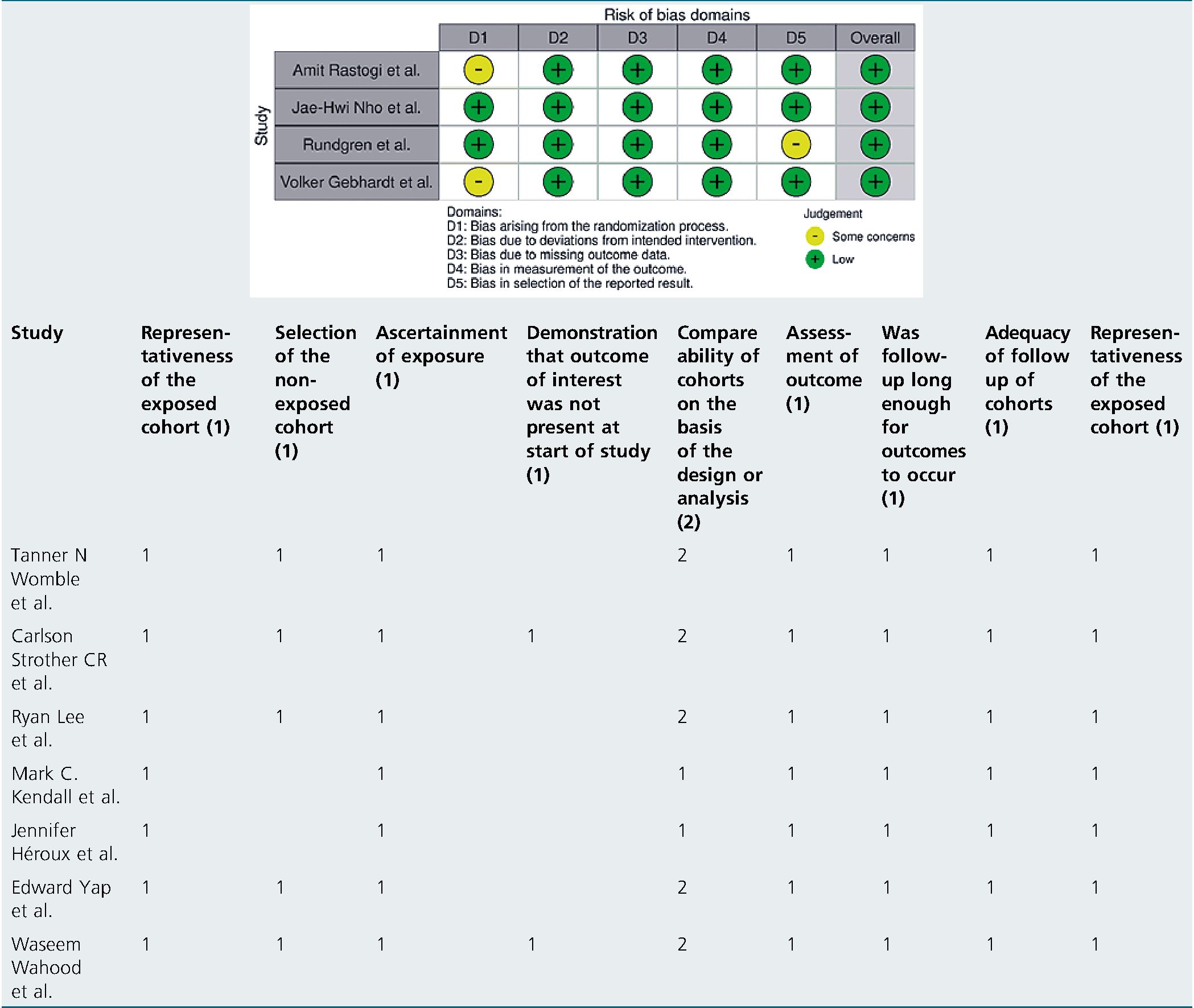
The quality of included studies is being assessed using appropriate tools such as the RoB 2.0 tool for randomized controlled trials and the Newcastle-Ottawa Scale for cohort studies.
-
Results
The characteristics and findings of the studies reviewed are narrated in Table 1. A total of 12 papers were included in the comprehensive review of outcomes after surgery including various methods of anesthesia: 4 randomized controlled trials (RCTs), 1 mixed-method observational research, and 7 cohort studies. Through the analysis of data from large patient groups having surgery under either regional anesthesia (RA) or general anesthesia (GA), the retrospective cohort studies offered insightful information. Numerous surgical techniques were covered by this research, such as lumbar decompression, total knee arthroplasty (TKA), ambulatory hip or knee arthroplasty, distal radius fracture surgery, ulnar nerve decompression, and ankle fracture surgery (Table 2).
Table 1. Characteristics and findings of the studies reviewed
The three randomized controlled trials (RCTs) assessed the effects of various anesthetic types on treatments, including volar plating for distal radius fractures, outpatient knee arthroscopy, and maxillofacial surgery. The controlled comparisons between RA and GA provided by these studies helped researchers get a better understanding of the effectiveness and safety of both anesthetic techniques. To evaluate day surgery patients’ postoperative recovery experiences and quality, a mixed-method observational research including qualitative and quantitative data was conducted. The studies covered a variety of participant groups having different surgical procedures, and their sample sizes ranged from a few hundred (minimum: 50) to several thousands (maximum: 353,970).
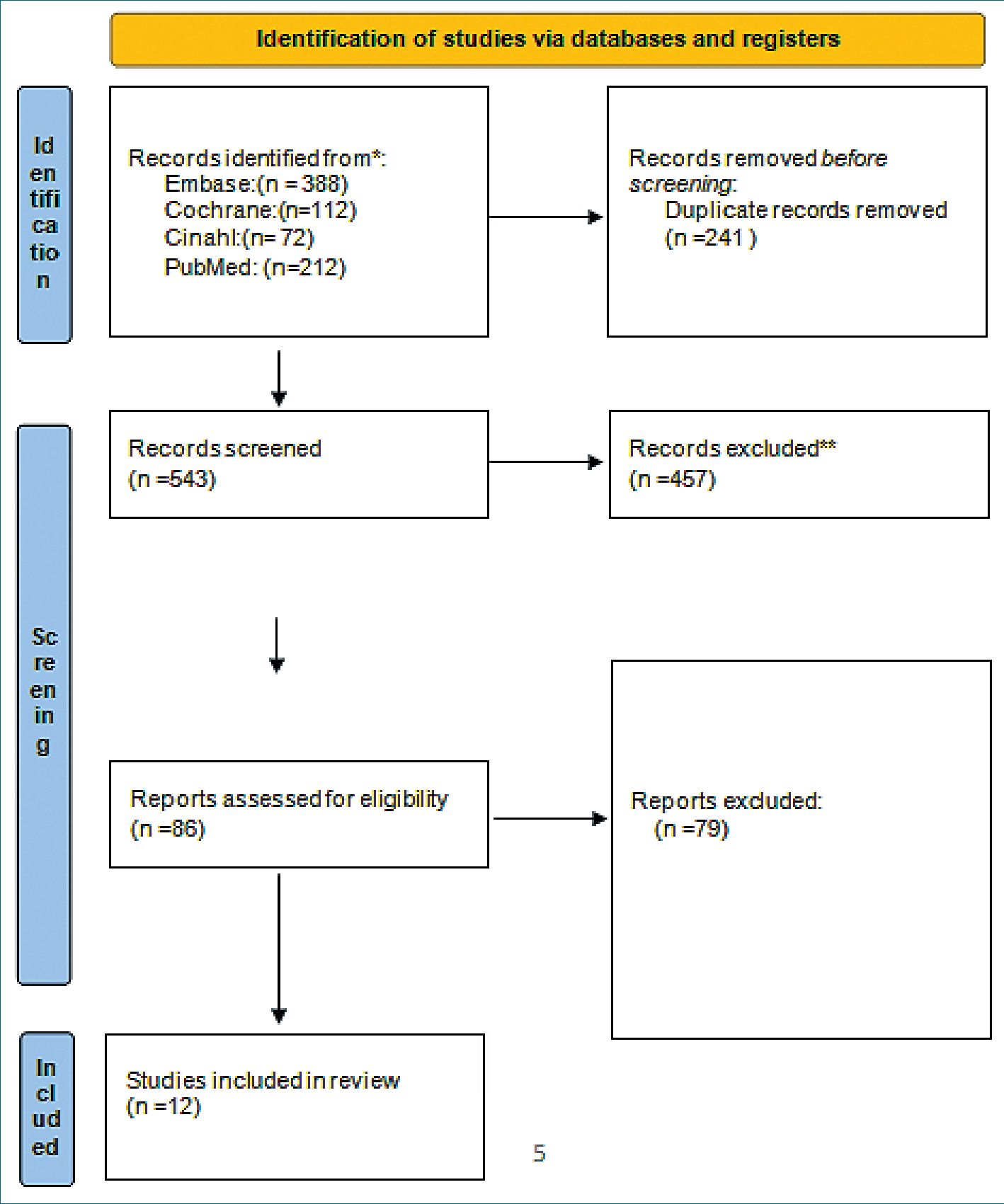
Figure 1. Prima flow diagram.
Evaluating postoperative outcomes, including surgery timeframes, complications, pain management, recovery times, readmissions, and functional recovery, was the main goal of the 12 trials. Some studies revealed no significant differences between the two anesthesia techniques, while others indicated benefits of RA over GA in some situations, such as less discomfort and shorter hospital stays. All things considered, the research offers significant understanding of the relative safety and efficacy of RA and GA in various surgical situations.
-
Discussion
In ambulatory traumatic procedures, the evaluated studies provide insightful information about the relative benefits of general anesthesia (GA) and regional anesthesia (RA). When choosing the best anesthesia method for a patient, it is important to carefully assess the benefits and limits of each technique. These studies support each other.
Based on the collective data from 12 studies, it can be concluded that, in ambulatory traumatic procedures, regional anesthesia (RA) typically provides better results than general anesthesia (GA). Research shows that RA is useful in a variety of surgical contexts, such as ankle fractures, lumbar decompression, and ulnar nerve decompression. Studies by Womble et al, Lee et al., Carlson Strother et al, and Wahood et al, consistently show this association with shorter hospital length of stay (LOS), comparable safety profiles, and lower rates of postoperative complications[6],[9],[8],[17]. Furthermore, RA is better than GA in terms of postoperative pain management and recovery, especially in maxillofacial and distal radius fracture procedures shown by Rastogi et al., and Nho et al.[12],[13]. These findings are supported by several research. Collectively, these results point to the possibility that RA might be a safer and more successful option than GA for ambulatory traumatic procedures, offering patients improved functional outcomes and pain management.
Table 2. Quality assessment of RCTs
Even as RA has several benefits, the data also shows that, in certain surgical procedures, there are no appreciable differences between GA and RA, or even possible benefits. Research by Nilsson et al., Kendall et al, and Gebhardt et al. indicates that decisions on RA vs GA may not have a major effect on how well patients recover after procedures including day surgery, outpatient total knee arthroplasty (TKA), and knee arthrosco- py[7],[10],[15]. Further evidence of similar results between the two anesthetic methods comes from Héroux et al., who found no discernible difference in functional recovery between the RA and GA groups after wrist surgery[11]. According to Yap et al., there were variations in pain management and postoperative nausea and vomiting (PONV), but overall, GA and neuraxial anesthesia (NA) produced comparable major complication rates in ambulatory hip or knee arthroplasty [16].
Different recovery patterns for GA and RA have been seen in several investigations, which is a consistent result. Patients having surgery under GA had worse recovery outcomes than those under RA, according to Ulrica Nilsson et al. [7]. These patients also reported higher levels of weariness and psychiatric problems. For outpatient knee arthroscopy, Volker Gebhardt et al., discovered that spinal anesthesia with 1% chloroprocaine led to a much quicker discharge and cheaper expenditures than GA[15]. When selecting an anesthesia approach for ambulatory operations, our results emphasize the need to take the patient’s comfort and recovery time into account.
But patients’ unique surgical needs and preferences should also be taken into account when deciding between GA and RA. Jennifer Heroux et al., for example, showed no appreciable difference in functional recovery between the RA and GA groups after wrist surgery for distal radial fractures [11]. It is possible that the kind of anesthesia used during an operation won’t have a major effect on the functional results in the long run.
The research is conflicting on safety and complication rates. Studies like Waseem Wahood et al, [17] and Carlson Strother CR et al,[8] observed no statistically significant difference in post-operative complications between the GA and RA groups, but Tanner N. Womble et al, found that the RA group had greater readmission rates for pain[6]. The disparity highlights the need for more investigation to get a deeper comprehension of the elements influencing post-operative problems and readmissions in ambulatory traumatic procedures.
Additionally, the results imply that when selecting the anesthesia approach, certain patient characteristics and preferences should be considered. In patients having surgery for distal radius fractures, for instance, Ryan Lee et al, discovered that RA may be recommended over GA since it was not linked to an increased risk of complications. The patients had high cardiac risk factors [9].
The variability of included studies with regard to anesthesia methods, surgical procedures, and outcome measures is one of the systematic review’s limitations since it may restrict how broadly the results can be applied. Furthermore, certain studies’ quality and design-such as those of retrospective cohort studies-may add bias and compromise the validity of the findings. Prospective viewpoints have to concentrate on carrying out meticulously planned randomised controlled trials with uniform procedures to contrast GA and RA in particular ambulatory trauma operations. Furthermore, studies examining characteristics unique to each patient, such comorbidities and preferences, may be able to better customise anesthetic techniques. In ambulatory traumatic operations, integrating cutting-edge technology like perioperative monitoring tools and enhanced recovery after surgery (ERAS) protocols may further optimize anesthesia management and improve patient recovery.
-
Conclusion
Finally, a thorough comparison of the results of general anesthesia (GA) vs regional anesthesia (RA) in ambulatory traumatic procedures is provided by this systematic review. Based on a comprehensive analysis of twelve trials covering a range of orthopedic operations and surgical methods, we have determined that both GA and RA are reasonable choices for anesthesia in ambulatory settings, with unique benefits and drawbacks. While some research revealed advantages of RA, such as decreased opioid use, shorter hospital stays, and less pain after surgery, other studies found similar results with GA and RA. The intricacy of the surgery, the patient’s features, and the postoperative recovery objectives all influence the choice of anesthesia. In order to improve clinical decision-making and patient outcomes in ambulatory settings, further research is required to clarify the best anesthesia strategy for certain ambulatory traumatic procedures.
-
References
1. Pace D, Hounsell C, Boone D. Ambulatory surgery centres: a potential solution to a chronic problem. Can J Surg [Internet]. 2023 Mar 17 [cited 2024 Apr 12];66[2]:E111. Available from: https://doi.org/10.1503/cjs.008022.
2. Folino TB, Mahboobi SK. Regional Anesthetic Blocks. StatPearls [Internet]. 2023 Jan 29 [cited 2024 Apr 12]; Available from: https://www.ncbi.nlm.nih.gov/books/NBK563238/
3. Roh YH, Park SG, Lee SH. Regional versus General Anesthesia in Postoperative Pain Management after Distal Radius Fracture Surgery: Meta-Analysis of Randomized Controlled Trials. Journal of Personalized Medicine [Internet]. 2023 Oct 27;13(11):1543. Available from: http://dx.doi.org/10.3390/jpm13111543
4. Smith G, D’Cruz JR, Rondeau B, Goldman J. General Anesthesia for Surgeons. StatPearls [Internet]. 2023 Aug 5 [cited 2024 Apr 12]; Available from: https://www.ncbi.nlm.nih.gov/books/NBK493199/
5. Mufarrih SH, Qureshi NQ, Yunus RA, Katsiampoura A, Quraishi I, Sharkey A, et al. A systematic review and meta-analysis of general versus regional anesthesia for lower extremity amputation [Internet]. J Vasc Surg. 2023 May;77(5):1542–1552.e9. [cited 2024 Apr 12] Available from: https://pubmed.ncbi.nlm.nih.gov/36243265/ https://doi.org/10.1016/j.jvs.2022.10.005 PMID:36243265
6. Womble TN, Comadoll SM, Dugan AJ, Davenport DL, Ali SZ, Srinath A, et al. Is supplemental regional anesthesia associated with more complications and readmissions after ankle fracture surgery in the inpatient and outpatient setting? [Internet]. Foot Ankle Surg. 2021 Jul;27(5):581–7. [cited 2024 Apr 12] Available from: https://pubmed.ncbi.nlm.nih.gov/32917527/ https://doi.org/10.1016/j.fas.2020.07.015 PMID:32917527
7. Nilsson U, Jaensson M, Dahlberg K, Hugelius K. Postoperative Recovery After General and Regional Anesthesia in Patients Undergoing Day Surgery: A Mixed Methods Study. Journal of PeriAnesthesia Nursing [Internet]. 2019 Jun;34(3):517–28. Available from: http://dx.doi.org/10.1016/j.jopan.2018.08.003
8. Carlson Strother CR, Dittman LE, Rizzo M, Moran SL, Rhee PC. Safety of Cubital Tunnel Release Under General versus Regional Anesthesia. Local and Regional Anesthesia [Internet]. 2023 Jul;Volume 16:91–8. Available from: http://dx.doi.org/10.2147/lra.s389011
9. Lee R, Lee D, Ramamurti P, Fassihi S, Heyer JH, Stadecker M, et al. Complications following regional anesthesia versus general anesthesia for the treatment of distal radius fractures [Internet]. Eur J Trauma Emerg Surg. 2022 Dec;48(6):4569–76. [cited 2024 Apr 12] Available from: https://pubmed.ncbi.nlm.nih.gov/34050773/ https://doi.org/10.1007/s00068-021-01704-1 PMID:34050773
10. Kendall MC, Cohen AD, Principe-Marrero S, Sidhom P, Apruzzese P, De Oliveira G. Spinal versus general anesthesia for patients undergoing outpatient total knee arthroplasty: a national propensity matched analysis of early postoperative outcomes [Internet]. BMC Anesthesiol. 2021 Sep;21(1):226. [cited 2024 Apr 12] Available from: https://link.springer.com/articles/10.1186/s12871-021-01442-2 https://doi.org/10.1186/s12871-021-01442-2 PMID:34525959
11. Héroux J, Bessette PO, Bédard S, Lamarche D, Gagnon A, Échavé P, et al. Récupération fonctionnelle après une chirurgie du poignet réalisée sous anesthésie régionale ou générale : une étude observationnelle prospective. Canadian Journal of Anesthesia/Journal canadien d’anesthésie [Internet]. 2023 Nov 6;71(6):761–72. Available from: http://dx.doi.org/10.1007/s12630-023-02615-y
12. Rastogi A, Gyanesh P, Nisha S, Agarwal A, Mishra P, Tiwari AK. Comparison of general anaesthesia versus regional anaesthesia with sedation in selected maxillofacial surgery: a randomized controlled trial. J Craniomaxillofac Surg. 2014 Apr;42(3):250–4. https://doi.org/10.1016/j.jcms.2013.05.010 PMID:23800753
13. Nho JH, Jang BW, An CY, Yoo JH, Song S, Cho HB, et al. General versus Brachial Plexus Block Anesthesia in Pain Management after Internal Fixation in Patients with Distal Radius Fracture: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health [Internet]. 2022 Jul 27;19(15):9155. Available from: http://dx.doi.org/10.3390/ijerph19159155
14. Rundgren J, Mellstrand Navarro C, Ponzer S, Regberg A, Serenius S, Enocson A. Regional or General Anesthesia in the Surgical Treatment of Distal Radial Fractures: A Randomized Clinical Trial [Internet]. J Bone Joint Surg Am. 2019 Jul;101(13):1168–76. [cited 2024 Apr 12] Available from: https://journals.lww.com/jbjsjournal/fulltext/2019/07030/regional_or_general_anesthesia_in_the_surgical.6.aspx https://doi.org/10.2106/JBJS.18.00984 PMID:31274718
15. Gebhardt V, Zawierucha V, Schöffski O, Schwarz A, Weiss C, Schmittner MD. Spinal anaesthesia with chloroprocaine 1% versus total intravenous anaesthesia for outpatient knee arthroscopy: A randomised controlled trial [Internet]. Eur J Anaesthesiol. 2018 Oct;35(10):774–81. [cited 2024 Apr 12] Available from: https://pubmed.ncbi.nlm.nih.gov/29521661/ https://doi.org/10.1097/EJA.0000000000000794 PMID:29521661
16. Yap E, Wei J, Webb C, Ng K, Behrends M. Neuraxial and general anesthesia for outpatient total joint arthroplasty result in similarly low rates of major perioperative complications: a multicentered cohort study [Internet]. Reg Anesth Pain Med. 2022 May;47(5):294–300. [cited 2024 Apr 12] Available from: https://rapm.bmj.com/content/47/5/294 https://doi.org/10.1136/rapm-2021-103189 PMID:34992150
17. Wahood W, Yolcu Y, Alvi MA, Goyal A, Long TR, Bydon M. Assessing the differences in outcomes between general and non-general anesthesia in spine surgery: results from a national registry. Clin Neurol Neurosurg. 2019 May;180:79–86. https://doi.org/10.1016/j.clineuro.2019.03.021 PMID:30952035

 ORCID
ORCID