Sherif S Sultan 1 , Nouran Mohsen Ahmed Fahmy 1 , Mohamed Ibrahim Hassan 1 , Dalia Fahmy Emam 1
Recibido: 02-07-2020
Aceptado: 17-08-2020
©2020 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 49 Núm. 6 pp. 889-895|https://doi.org/10.25237/revchilanestv49n06-15
PDF|ePub|RIS
Pack orofaringeo con triamcinolone disminuye molestias luego de cirugía endoscópica sinusal
Abstract
background: Postoperative sore throat (POST) is defined as pain or discomfort in the throat following general anesthesia. Throat packs are used by many surgical subspecialties for different benifits, however they may increase the incidence of POST. Many interventions can be used to decrease incidence of POST. Triamcinolone acetonide (TA) is a moderately potent topical corticosteroid preparation. In this study, we hypothesized that soaking the throat pack with TA may decrease POST. Methods and Material: This prospective interventional comparative study was performed on 54 patients planned for Functional Endoscopic Sinus Surgeries (FEES) surgery. After endotracheal intubation, a standard length of oro-pharyngeal pack was placed, then patients were randomly allocated into: Group I: Oro-pharyngeal packs were soaked with 15 mg Triamcinolone acetonide 0.1% and Group II: packs were soaked with the same volume of lubricating gel (K-Y gel®). The patients were postoperatively asked about: sore throat, dysphagia, hoarseness of voice and nausea and vomiting. Results: Thirty minutes and 24 hours after extubation, Group I patients showed lower but statistically insignificant sore throat scores. Two to six hours after extubation, Group I showed a statistically significant reduction in sore throat scores. Six patients suffered dysphagia in group I compared with 8 patients in group II. Hoarseness of voice occurred in 1 patient in group I and 3 patients in group II. No patient complained of nausea or vomiting. Conclusión: Soaking oropharyngeal pack with triamcinolone acetonide in orabase gel was able to decrease POST in FESS patients.
-
Introduction
Postoperative sore throat (POST) is defined as pain, discomfort, scratchiness or irritation in the throat following general anesthesia that always worsens with swallowing. It may be due to pharyngitis or laryngitis. Highest incidence is after tracheal intubation (14.4%-64%)[1],[2] followed by after insertion of laryngeal mask airway (LMA) (4.1%-34%) [3],[4]. It is believed to occur even after general anesthesia based on face mask application[ 5 ]. Insertion of simple airway devices e.g. oropharyngeal or nasopharyngeal airway may also share its occurrence and increase its severity[ 6 ].
Throat packs are used by many surgical subspecialties for different reasons. They collect blood, secretions, bony and cartilaginous debris intraoperatively. This is claimed to decrease their inhalation and swallowing postoperatively and therefore decrease the incidence of postoperative complications e.g. postoperative nausea and vomiting[ 7 ]. Whatever were the benefits behind the insertion of throat packs they still have their side effects. Between these side effects is increasing the incidence of POST[ 8 ].
Many interventions can be used to decrease incidence of POST. These include using smaller endotracheal tube size[9] including video laryngoscopy in intubation process[10], limiting endotracheal cuff pressure[11], perioperative use of steroids (intravenous[12], topical[13] or inhaled[14 ]), the use of topical non-steroidal anti-inflammatory drugs (NSAIDs) [15] and the use of different gargles (magnesium and ketamine[16].
Triamcinolone acetonide (TA) is a moderately potent corticosteroid preparation that is commonly used in wide range of oral mucosal lesions. These include different inflammatory and immunological lesions such as recurrent aphthous stomatitis[17 ] and oral lichen planus[18]. It has been used successfully to decrease POST when applied along the length of the ETT[ 13 ]. Considering that application of throat pack may increase the incidence of POST, we hypothesized that the use of TA when added as an ora-base gel to the throat pack may decrease POST.
-
Methods
This prospective interventional comparative study was performed after approval of Research Ethics Committee, Faculty of Medicine, Ain Shams University, and Cairo, Egypt (FMASU M S 49/2019) and registered at Pan African Clinical Trial Registry (www. pactr.org, PACTR201909823246718). The study was performed at Ain Shams Universities Hospitals, Cairo, Egypt. Written informed consent was obtained from all patients prior to performing the procedure.
Patients undergoing Functional Endoscopic Sinus Surgeries (FESS) where enrolled in this double-blinded, randomized, controlled trial. Inclusion criteria included patient’s age between 18 and 60 years, American Society of Anesthesiologists (ASA) physical status classification system class I and II, modified Mallampatti classification I and II, with no significant preexisting laryngotracheal diseases other than the indication of surgery. Patients included were presumed to undergo an easy intubation and a duration of surgery of less than 3 hours. Exclusion criteria included pharyngeal infection or ulceration, smokers, patients on corticosteroids or NSAIDs.
After arrival to the operating theatre, patients were attached to the monitors as per standard protocols. The same standardized anesthesia technique was used for all patients which included induction with fentanyl (1 pg/kg), propofol (2 mg/kg) and atracurium (0.5 mg/kg) and maintenance with 1.5-2% isoflurane in O2/Air mixture. Another booster dose of fentanyl (1 pg/kg) was given at start of surgery and top-up doses of atracurium were used according to the attending anesthesiologist. Endotracheal intubation was performed using disposable, well-lubricated tubes with an internal diameter of 7 mm for females and 7.5 mm for males. Endotracheal tube cuffs were inflated with air to reach a pressure of 25 mmHg. Patients requiring more than one attempt for passage of the tube were excluded from the study.
A standard length of oro-pharyngeal pack 120 cm and a width of 7.5 cm was placed under direct vision using Magill forceps and positioned in the oropharynx, thus isolating the nasal passage in order to allow suctioning of blood and debris from the operative field and prevent soiling of the pharynx, oesophagus and tracheal contamination. A label on the patient’s forehead or the airway device was applied, and the time of insertion and removal of the oral pack was recorded on the operating room white board and the anesthetic sheet to avoid the risk of leaving the pack accidently in place after extubation.
At this point, patients were randomly allocated into one of two groups utilizing computer generated list for allocation; Group I “Study Group”: Oro-pharyngeal packs were soaked with addition of 15 mg Triamcinolone acetonide 0.1% (Kenacort Orabase gel, SmithKline Beecham, London, UK) or Group II “Control Group”: Oro-pharyngeal packs were soaked with addition of the same volume of lubricating gel (K-Y gel®) for blinding. The soaked pack was positioned by residents blinded to the gel used to moisten the throat pack.
Patients were placed in a head-up position in order to provide optimum conditions for the surgery. If hypotensive anesthesia was needed, glyceryl trinitrate was used avoiding use of opioids, propranolol or increasing the concentration of inhaled anesthetic. At the end of operation, oro-pharyngeal pack was removed, and IV paracetamol (1 gm) was given. The nose was closed by a small nasal packing. Oropharyngeal suction before extubation was done under direct vision with a suction catheter, confirming that secretion clearance was complete. After completion of surgical procedure duration of surgery was recorded.
Postoperatively, patients who were unaware of which gel had been used, were interviewed by a blinded investigator and asked about 4 complaints; sore throat, difficulty in swallowing (dysphagia), hoarseness of voice and postoperative nausea and vomiting. For sore throat, it was determined at the following intervals: 30 min after extubation, 2-6 hours after extubation and 24 hours after extubation. It was categorized based on visual analogue scale. The other 3 complaints were categorized as yes or no 24 h after extubation. All patients received oral paracetamol (500 mg/6 hours) postoperatively.
Sample size was calculated according to Chandak et al. study (2017) in which 0.1% triamcinolone acetonide paste succeeded in decreasing pain secondary to aphthous stomatitis from 3.60 ± 1.502 to 2.13 ± 1.302 in 24 h. Therefore, 16 patients per group would be sufficient to give 80% power at a 5% significance level. We enrolled 27 patients in each group.
Data were analyzed using Statistical Package for Social Science (SPSS Inc., Chicago, IL, USA, version 23.0 for windows). The quantitative parametric data were presented as mean, standard deviations (SD) and ranges then compared using independent t-test. The quantitative nonparametric data were presented as median, inter-quartile range (IQR) then compared using Mann-Whitney U-test. Qualitative variables were presented as number and percentages then compared with Chi-square test. The confidence interval was set to 95% and the margin of error accepted was set to 5%. Accordingly, the p-value was considered statistically significant when < 0.05.
| Table 1. Comparison between the two groups regarding age, sex and duration of surgery+ | |||
| Group I | Group II | P-value | |
| Age in years (Mean ± SD) | 29.81 ± 5.53 | 30.81 ± 6.87 | 0.558 |
| Sex (Female/male) | 13/14 | 7/20 | 0.091 |
| Duration of surgery (hours) (Mean ± SD) | 2.21 ± 0.15 | 2.21 ± 0.15 | 0.929 |
Fifty-four patients were included in the study equally divided into two groups. No significant differences were detected between the two groups concerning age, sex and duration of surgery (Table 1). Median scores of sore throat are shown in Table 2. Thirty minutes and 24 hours after extubation, Group I patients showed lower sore throat scores but that were statistically insignificant. Two to six hours after extubation, Group I showed a statistically significant reduction in sore throat scores compared to Group II (control group). This is shown in Figure 1.
A total of 6 patients suffered dysphagia in group I compared with 8 patients in group II with statistically insignificant difference. Hoarseness of voice was a complain of 1 patient in group I and 3 patients in group II with a statistically insignificant result. No patient complained of nausea or vomiting in our study (Table 3).
| Table 2. Comparison between the two groups regarding sore throat at 30 mins, 2-6 h and 24 h post-extubation. Data are presented as median (IQR) | |||
| Sore throat | Group I | Group II | P-value |
| 30 min | 4 (4 – 5) | 5 (4 — 6) | 0.360 |
| 2-6 h | 3 (3 — 4) | 4 (3 — 4) | 0.028 |
| 24 h | 1 (1 — 2) | 2 (1 — 2) | 0.306 |
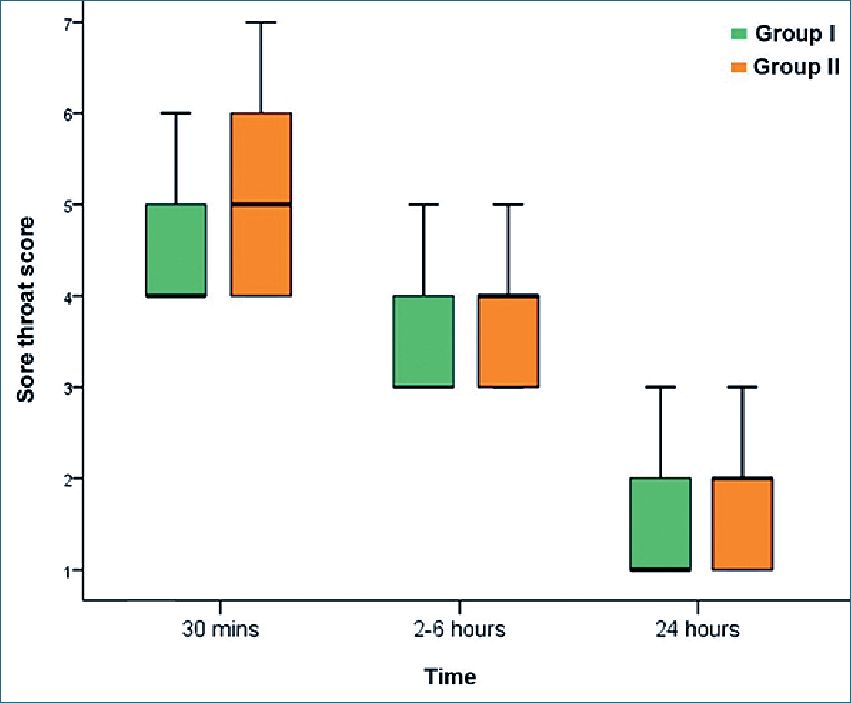
Figure 1. Sore throat scores at 30 mins, 2-6 hours and 24 hours post-extubation. Data are presented as median (IQR).
Postoperative sore throat is a common anesthetic complication that is considered by many anesthesiologists as a minor complication. However, it may be the first complain for some patients immediately after getting their conscious back even before they may complain of the incisional/operative pain. It should be avoided and prevented better than treating it. Prevention of POST is expected to improve the patient satisfaction and comfort postoperatively. Moreover, prevention is expected to reduce the patient stay in PACU and the overall hospital stay[19 ]dislodgement or (partial especially in day-surgery cases.
The use of oropharyngeal pack is a common practice asked by surgeons of different surgical sub-specialties. These include dental, oral and maxilofacial surgeries, a wide variety of rhino-pharyngo-laryngeal surgeries and neurosurgical surgeries that involve nasal route. It is well known that the use of pharyngeal packs adds to the postoperative discomfort and pain [20][8]. The mechanism behind POST caused by oropharyngeal packs is not very well-understood. An oropharyngeal pack may induce POST by the process of packing itself. Packing may include pharyngeal instrumentation (using laryngoscopy and/or Magill forceps) and passage of the hard, abrasive fibers (especially if not fully soaked) of cotton texture in its way from the incisors to its destination in oro-pharynx. This passage is performed through the oral cavity which is considered a pit tight canal that differs from person to person. Insertion of the oro-pharyngeal pack may induce dryness of the adjacent tissues through suction of water and body fluids by this dry piece of texture. This dryness may induce an area that is ready for inflammation. It is well-known that manipulation of abdominal towels containing cotton is associated with development of peritoneal adhesions[ 21 ]. Accordingly, it is not very strange that cotton fibers itself may induce inflammatory process for an adjacent mucosal surface.
In the current study, duration of surgery was 2.2 hours. Accordingly, it may be concluded that asking the patient about POST 30 minutes after extubation is about 3 hours after inserting the oro-pharyngeal pack. It is not known exactly the onset of action of topical steroids. Pharmacokinetics of topical steroids (including that in Ora-base forms) are affected by potency of the preparation, amount applied, nature of area applied to (thick skin, thin skin or mucosa) and condition of area applied to (normal, ulcerated or inflamed)[22 ]. It seems that 3 hours were not enough for triamcinolone acetonide to have its full effects that can decrease throat pain secondary to throat pack immediately postoperatively. The causative factors for POST after 30 mins other than throat packs may have been prevalent at that time. These factors may include lack of airway humidity, trauma during airway insertion, suctioning, high anesthetic gas flow rates and surgical manipulation of airway and adjacent tissue[23 ]. These factors may be the cause that our results showed decrease in POST 30 minutes after extubation but failed to reach statistical significance.
| Table 3. Comparison between the two groups regarding dysphagia, hoarseness and nausea and vomiting. Data are presented as number of patients | |||
| Group I | Group II | P-value | |
| Dysphagia (No/Yes) | 21/6 | 19/8 | 0.535 |
| Hoarseness (No/Yes) | 26/1 | 24/3 | 0.299 |
| Nausea and vomiting (No/Yes) | 27/0 | 27/0 | — |
However, 2-6 hours postoperatively, effects of triamcinolone acetonide in decreasing POST due to oro-pharyngeal pack were evident. During this time, pain scores were significantly lower in study group compared to control group. This may be attributed to reaching the maximum available effect of topical triamcinolone acetonide applied. Triamcinolone acetonide is able to decrease number and functions of different inflammatory cells at site of inflammation including T and B lymphocytes, neutrophils, monocytes and eosinophils. Moreover, production of cytokines, chemokines, eicosanoids is markedly inhibited while the production of macrophage migration inhibitory factor is markedly enhanced[ 24 ].
After 24 hours, POST declines progressively to the degree that it is difficult to elicit the effect of the study drugs except, perhaps, if we have a bigger sample size. This generally goes with the usual noticed nature of behavior of POST that it usually subsides in most of patients by the end of the first postoperative day even without any extra analgesic more that the usually used postoperative analgesics[25 ]. An exception is the rough airway manipulation during a difficult intubation scenario.
The use of corticosteroids in prophylaxis against or treatment of POST is previously documented. A meta-analysis performed by[26 ] recommended that IV dexamethasone should be used in reduction of POST, hoarseness and PONV as grade 1A of evidence in a dose > 0.2 mg/kg in patients who are not pregnant, diabetic or have contraindications to corticosteroids. Moreover, gargling preoperatively with 0.05% dexamethasone decrease POST incidence from 63% to 33% when compared with gargling with normal saline[27 ].
The current study proved no statistically different results between the study group and the control group concerning dysphagia and hoarseness of voice. Dysphagia and hoarseness of voice were reported in the current study 24 hours after extubation. At that time, POST were not statistically different between the groups. As mentioned above, TA effects may have been faded away. Results in the current study concerning PONV go in line with other studies who proved no association between pharyngeal packs and PONV[28],[8],[20]. Adding to this is that topically applied TA is not expected to affect this kind of postoperative complication.
There are few limitations of this current study. First is that the sample size is low and if a bigger sample size was used the effects of topically applied triamcinolone acetonide may have a statistically significant results 30 minutes and 24 hours after extubation. Second is that the current study ignored the possible effects of systemically absorbed triamcinolone acetonide. This comes in concern when studies prove that systemically applied corticosteroids can decrease severity of POST[ 27 ]. However, Ramadas et al. proved that no systemic absorption is expected from topically TA applied to oral mucosa reflecting its safety profile[18 ].
In conclusion, soaking oropharyngeal pack with triamcinolone acetonide in ora-base gel was able to decrease POST in FESS patients.
-
References
1. Christensen AM, Willemoes-Larsen H, Lundby L, Jakobsen KB. Postoperative throat complaints after tracheal intubation. Br J Anaesth. 1994 Dec;73(6):786–7. https://doi.org/10.1093/bja/73.6.786 PMID:7880666
2. Obiaya M, Okechukwu C, Dakaraju P, et al. The incidence of post anaesthetic complications-a follow-up programme. West Afr J Med. 1984;3:165–9.
3. Wakeling HG, Butler PJ, Baxter PJ. The laryngeal mask airway: a comparison between two insertion techniques. Anesth Analg. 1997 Sep;85(3):687–90. https://doi.org/10.1213/00000539-199709000-00037 PMID:9296432
4. Joshi GP, Inagaki Y, White PF, Taylor-Kennedy L, Wat LI, Gevirtz C, et al. Use of the laryngeal mask airway as an alternative to the tracheal tube during ambulatory anesthesia. Anesth Analg. 1997 Sep;85(3):573–7. https://doi.org/10.1213/00000539-199709000-00016 PMID:9296411
5. Dingley J, Whitehead MJ, Wareham K. A comparative study of the incidence of sore throat with the laryngeal mask airway. Anaesthesia. 1994 Mar;49(3):251–4. https://doi.org/10.1111/j.1365-2044.1994.tb03434.x PMID:8147523
6. Gemechu BM, Gebremedhn EG, Melkie TB. Risk factors for postoperative throat pain after general anaesthesia with endotracheal intubation at the University of Gondar Teaching Hospital, Northwest Ethiopia, 2014. Pan Afr Med J. 2017 Jun;27:127. https://doi.org/10.11604/pamj.2017.27.127.10566 PMID:28904657
7. Fennessy BG, Mannion S, Kinsella JB, O’Sullivan P. The benefits of hypopharyngeal packing in nasal surgery: a pilot study. Ir J Med Sci. 2011 Mar;180(1):181–3. https://doi.org/10.1007/s11845-010-0601-4 PMID:21110138
8. Karbasforushan A, Hemmatpoor B, Makhsosi BR, Mahvar T, Golfam P, Khiabani B. The effect of pharyngeal packing during nasal surgery on the incidence of postoperative nausea, vomiting, and sore throat. Iran J Otorhinolaryngol. 2014 Oct;26(77):219–23. PMID:25320699
9. Hu B, Bao R, Wang X, Liu S, Tao T, Xie Q, et al. The size of endotracheal tube and sore throat after surgery: a systematic review and meta-analysis. PLoS One. 2013 Oct;8(10):e74467. https://doi.org/10.1371/journal.pone.0074467 PMID:24124452
10. Najafi A, Imani F, Makarem J, Khajavi MR, Etezadi F, Habibi S, et al. Postoperative sore throat after laryngoscopy with macintosh or glide scope video laryngoscope blade in normal airway patients. Anesth Pain Med. 2014 Feb;4(1):e15136. https://doi.org/10.5812/aapm.15136 PMID:24660157
11. Ansari L, Bohluli B, Mahaseni H, Valaei N, Sadr-Eshkevari P, Rashad A. The effect of endotracheal tube cuff pressure control on postextubation throat pain in orthognathic surgeries: a randomized double-blind controlled clinical trial. Br J Oral Maxillofac Surg. 2014 Feb;52(2):140–3. https://doi.org/10.1016/j.bjoms.2013.10.005 PMID:24268872
12. Sun L, Guo R, Sun L. Dexamethasone for preventing postoperative sore throat: a meta-analysis of randomized controlled trials. Ir J Med Sci. 2014 Dec;183(4):593–600. https://doi.org/10.1007/s11845-013-1057-0 PMID:24357270
13. Park SY, Kim SH, Lee SJ, Chae WS, Jin HC, Lee JS, et al. Application of triamcinolone acetonide paste to the endotracheal tube reduces postoperative sore throat: a randomized controlled trial. Can J Anaesth. 2011 May;58(5):436–42. https://doi.org/10.1007/s12630-011-9478-6 PMID:21359615
14. Tazeh-Kand NF, Eslami B, Mohammadian K. Inhaled fluticasone propionate reduces postoperative sore throat, cough, and hoarseness. Anesth Analg. 2010 Oct;111(4):895–8. https://doi.org/10.1213/ANE.0b013e3181c8a5a2 PMID:20237046
15. Chang JE, Min SW, Kim CS, Han SH, Kwon YS, Hwang JY. L’effet d’une prophylaxie de chlorhydrate de benzydamine sur les maux de gorge et l’enrouement postopératoires après une intubation trachéale à l’aide d’une sonde endobronchique à double lumière: une étude randomisée controlee. Can J Anaesth. 2015;62(10):1097–103. https://doi.org/10.1007/s12630-015-0432-x PMID:26149601
16. Teymourian H, Mohajerani SA, Farahbod A. Magnesium and ketamine gargle and postoperative sore throat. Anesth Pain Med. 2015 Jun;5(3):e22367. https://doi.org/10.5812/aapm.5(3)2015.22367 PMID:26161316
17. Shrivastava NG, Deshpande A, Handa H, Raghuvanshi V, Gupta M. Comparative evaluation of the efficacy of topical amlexanox 5% oral paste and triamcinolone acetonide 0.1% oral paste in the treatment of Recurrent Aphthous Stomatitis (RAS). J Indian Acad Oral Med Radiol. 2018;30(3):235.
18. Ramadas AA, Jose R, Arathy SL, Kurup S, Chandy ML, Kumar SP. Systemic absorption of 0.1% triamcinolone acetonide as topical application in management of oral lichen planus. Indian J Dent Res. 2016 May-Jun;27(3):230–5. https://doi.org/10.4103/0970-9290.186237 PMID:27411649
19. Smarius BJA, Guillaume CHAL, Jonker G, Mink Van Der Molen AB, and Breugem CC. The use of throat packs in pediatric cleft lip/palate surgery: a retrospective study. 2018; 22:3053-3059.
20. Basha SI, McCoy E, Ullah R, Kinsella JB. The efficacy of pharyngeal packing during routine nasal surgery—a prospective randomised controlled study. Anaesthesia. 2006 Dec;61(12):1161–5. https://doi.org/10.1111/j.1365-2044.2006.04868.x PMID:17090236
21. Liu BG, Ruben DS, Renz W, Santillan A, Kubisen SJ, Harmon JW. Comparison of peritoneal adhesion formation in bowel retraction by cotton towels versus the silicone lap pak device in a rabbit model. Eplasty. 2011;11:e42. PMID:22096614
22. Dhar S, Seth J, Parikh D. Systemic side-effects of topical corticosteroids. Indian J Dermatol. 2014 Sep;59(5):460–4. https://doi.org/10.4103/0019-5154.139874 PMID:25284850
23. Patil BO, Ravindra Sonavdekar S, Mathur R. A Relative Study on Laryngeal Mask Airway Lubrication with 0.005% Beclomethasone Cream v/a 2% Lidocaine. Orig. Res. Artic. 2019;206(3):206–15.
24. Gibson N, Ferguson JW. Steroid cover for dental patients on long-term steroid medication: proposed clinical guidelines based upon a critical review of the literature. Br Dent J. 2004 Dec;197(11):681–5. https://doi.org/10.1038/sj.bdj.4811857 PMID:15592544
25. Arta SA, Ghavimi MA, Rahbar M, Ali-Maddadi Y, Zarandi A. Effect of Pharyngeal Pack on Postoperative Nausea and Throat Pain in Patients Undergoing Rhinoplasty. Pesqui Bras Odontopediatria Clin Integr. 2019;19(1):1–8. https://doi.org/10.4034/PBOCI.2019.191.56.
26. Jiang Y et al. The impact of prophylactic dexamethasone on postoperative sore throat: An updated systematic review and meta-analysis. Journal of Pain Research. 2018; 11. Dove Medical Press Ltd: 2463–2475.
27. Lee JH, Kim SB, Lee W, Ki S, Kim MH, Cho K, et al. Effects of topical dexamethasone in postoperative sore throat. Korean J Anesthesiol. 2017 Feb;70(1):58–63. https://doi.org/10.4097/kjae.2017.70.1.58 PMID:28184268
28. Razavi M, Taghavi Gilani M, Bameshki AR, Behdani R, Khadivi E, Bakhshaee M. Pharyngeal Packing during Rhinoplasty: advantages and Disadvantages. Iran J Otorhinolaryngol. 2015 Nov;27(83):423–8. PMID:26788486

 ORCID
ORCID