Barry Friedberg1
Recibido: 02-05-2024
Aceptado: 12-05-2024
©2024 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 53 Núm. 4 pp. 322-326|https://doi.org/10.25237/revchilanestv53n4-05
PDF|ePub|RIS
Abstract
Friedberg’s Triad for opioid free anesthesia is a simple, minimally invasive paradigm which is 1) Measures the brain; 2) Preempt the pain; 3) Emetic drugs abstain. After an incremental propofol induction, ketamine 50 mg IV produces 10-20 minutes’ immobility for the surgeon’s tumescent analgesia injections. Immobility with the 50 mg dose was consistently observed in patients weighing between 80 to 146 kg. Processed EEG monitoring Immobility from the pain of tumescent anesthesia injections was eliminated with a unit ketamine does of 50 mg independent of weight or age.
La tríada de Friedberg y la anestesia sin opiáceos en el paciente con obesidad mórbida
Resumen
La tríada de Friedberg para la anestesia sin opiáceos es un paradigma sencillo, y mínimamente invasivo, que consiste en 1) Medir el cerebro; 2) Prevenir el dolor; 3) Abstenerse de fármacos eméticos. Tras una inducción incremental de propofol, la ketamina 50 mg IV se utilizó para producir inmovilidad de 10-20 minutos para las inyecciones de analgesia tumescente del cirujano. La inmovilidad con la dosis de 50 mg se observó consistentemente, en pacientes entre 80 a 146 kg. El EEG procesado monitorizó la inmovilidad del dolor de las inyecciones de anestesia tumescente que fue eliminado con ketamina de 50 mg, independientemente del peso o la edad.
Friedberg’s Triad in combination with regional anesthesia is a simplified propofol then ketamine paradigm for opioid free anesthesia (OFA) and better outcomes[1] (Figure 1). Other OFA paradigms involve more drugs[2],[3]. Friedberg’s Triad is 1) Measure the brain; 2) Preempt the pain; 3) Emetic drugs abstain. The BIS trend is delayed 15-30 seconds from real time. Titrating propofol with BIS trend only is akin to trying to drive a car with only the rear-view mirror information. Real time EMG trending greatly improves BIS utility.
Anesthesia may be defined as hypnosis plus analgesia. Hypnosis can include amnesia. Analgesia can include sufficient muscle relaxation to imbricate the rectus muscle sheath for abdominoplasty or dissect the pectoralis muscle off the chest wall for a submuscular breast augmentation. The surgical era of lengthy skin incisions for large thoracic or abdominal retractors belongs to the 20th century. The benefits of 21st century, minimally invasive surgery can be enhanced with minimally invasive anesthesia[4].
Prior to the 1998 addition of brain monitoring to this cosmetic surgery anesthesia practice, hypnosis was defined by incrementally titrating propofol to a loss of lid reflex and loss of verbal response. Hypnotic doses of propofol block ketamine hallucinations[5]. Additional advantages of an incremental propofol induction are avoiding creating the difficult airway[6] and rapid identification of the dramatic variation in propofol rates to achieve identical numerical sedation levels[7].
If you cannot measure it, you cannot improve it. -Lord Kelvin
Hypnosis can be reproducibly measured with bispectral (BIS) index monitoring. Moderate to deep sedation is 60<BIS<75. General anesthesia is 40 < BIS < 60[8]. Most patients can achieve 60 < BIS < 75 with propofol infusion rates between 2550 mcg ˑkg-1 ˑmin.-1 Very sensitive patients achieve 60 < BIS < 75 with a rate as low as 2 mcg ˑkg-1ˑmin-1 and very resistant patients may require a rate as high as 200 mcg ˑkg-1 ˑ minˑ– 1[7].
Directly measuring patient cortical response exposes this 100-fold variation in rates required to achieve identical sedation levels.
An incremental, not bolus, induction maintains baseline tone in the genioglossus, masseter, temporalis, and orbicularis oris muscles, maintaining a patent airway, spontaneous ventilation, and often, without requirement for supplemental oxygen. In this video clip (https://lnkd.in/gAnPtSD) the infusion pump was set to a 25 mcg ˑkg-1 ˑmin-1 baseline infusion rate while the patient received 50 mcg ˑkg-1 for each repeated bolus until the EMG showed its initial descent towards the baseline. Both the rate and bolus are adjusted according to the BIS and EMG response.
In the preceding YouTube video, neither a chin lift nor an artificial airway was required to maintain the airway. Despite no supplemental oxygen, the pulse oximeter tone is unchanged while the hypnosis level decreases to the desired BIS < 75 range with baseline, real time EMG. Incremental propofol induction provides a stable CNS level warding off ketamine hallucinations, hypertension, and tachycardia[1]. Elimination of opioids avoids compounding propofol respiratory depression as well as abetting spontaneous ventilation and preventing the difficult airway.
After an incremental propofol induction, ketamine 50 mg IV produces 10-20 minutes’ immobility for the surgeon’s tumescent analgesia injections. Immobility with the 50 mg dose was consistently observed in patients weighing between 30 to 146 kg and in ages 7 up to 94. The effective NMDA receptor saturating ketamine dose does not appear to vary with either weight or age[7]. Ketamine 50 mg is administered 2-3 minutes prior to tumescent analgesia injections.
Glycopyrrolate 0.2 mg is always administered prior to propofol induction to decrease secretions that may produce ketamine associated laryngospasm[9]. This type of laryngospasm involves the complete vocal cord closure without the characteristic ‘crowing’ sounds. Only a cough or sneeze may precede ketamine associated laryngospasm. Prompt recognition and treatment with 1 mgˑpound-1 or 2 mg ˑkg-1 IV lidocaine will resolve the issue[9].
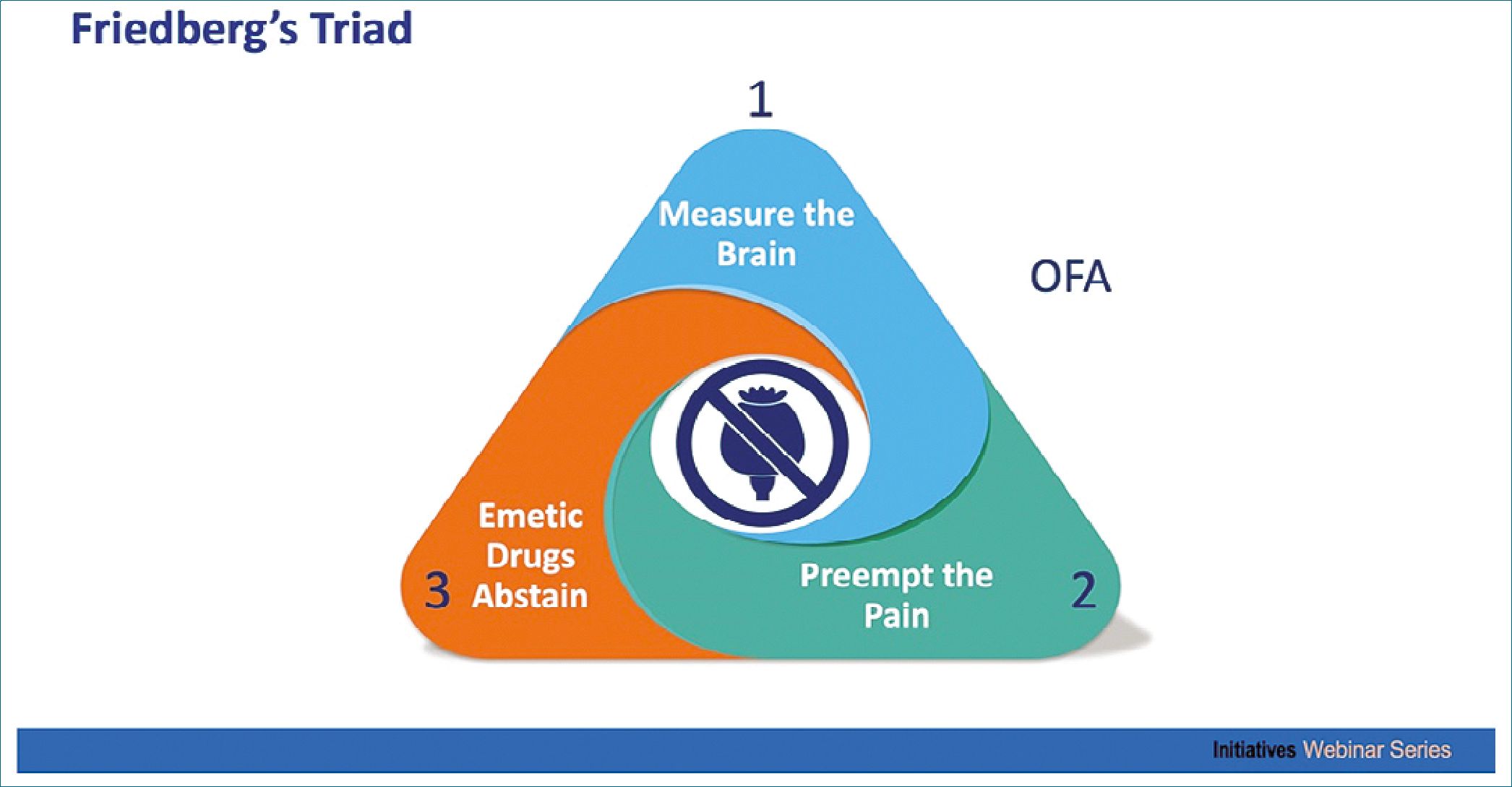
Figure 1. Friedberg’s Triad. The character in the middle of the Triad is an opium poppy.
While scientifically validated surveyed anesthesiologists chose pain as the ##1 outcome to avoid[10], patients chose emesis as #1, gagging on the ET #2, nausea #3, and pain as a surprising #4 outcome to avoid[11]. PONV is patients’ number one anesthesia outcome to avoid. PONV is a disconcerting outcome especially in cosmetic surgery as retching may disrupt rectus sheath sutures or produce a facial hematoma in rhytidectomy patients. A 0.6% PONV rate was published in an Apfel-defined high risk, opioid free, propofol then ketamine outpatient population without antiemetics[12] validating opioids as the principal cause of PONV[13]. Apfel wrote, ‘As long as emetogenic agents are part of the anesthetic regimen, the use of antiemetics is of limited utility[14].
Analgesia in cosmetic surgery is commonly administered with multiple, stimulating, percutaneous injections into the subcutaneous tissues by the surgeon with ultra-dilute or tumescent solution. Tumescent lidocaine analgesia has its practical limits. Klein published 35 mg ˑkg.-1 (15) with liposuction and 28 mg ˑ kg.-1 without liposuction[16]. Ostad published up to 55 mg ˑ kg.-1[17]. Tumescent volumes greater than 5,000 ccs of tumescent analgesia are associated with higher complication rates. As such, 5,000 ccs is considered an upper safe limit in California. In Florida, 4,000 ccs is considered to be the safe upper limit.
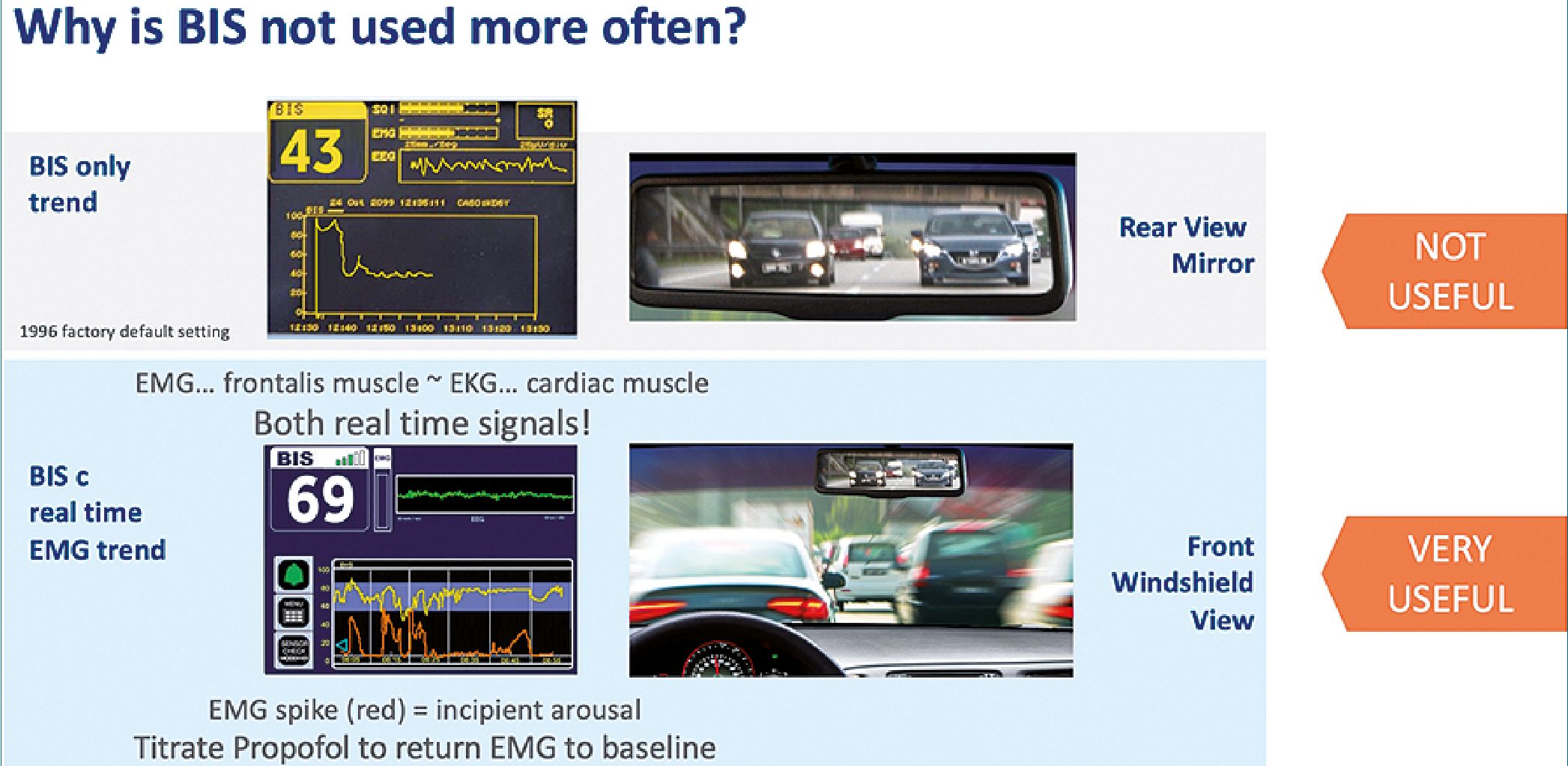
Figure 2. Why BIS is not used more often.
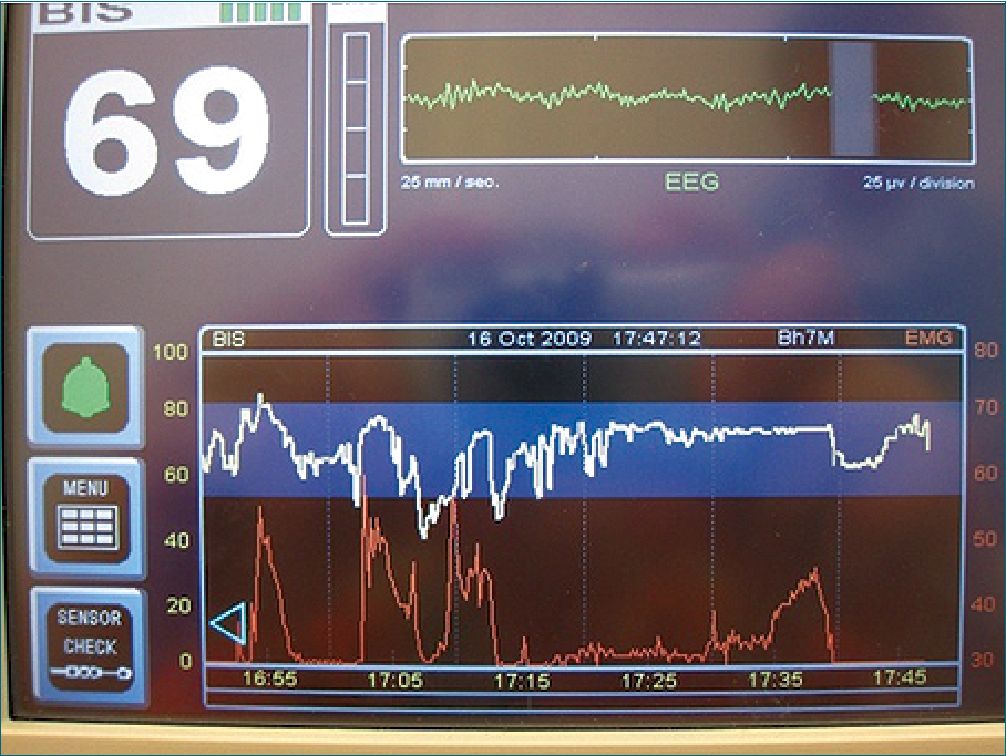
Figure 3. Free-standing BIS unit with lower (red) real time EMG trend. BIS trend is delayed from real time by 15-30 seconds.

Figure 4. Arousal precedes nociception… ‘Ouch’ precedes withdrawal.
The BIS trend is delayed from real time by 15-30 seconds. Figure 2 Unlike the plug-in modules, only free-standing BIS units allow the display of the real time EMG trend. This trend appears as the lower (red) line. Figure 3 EMG spikes signal incipient arousal[18]. Arousal precedes nociception. Ouch precedes withdrawal. Figure 4 Responding to EMG spikes with sufficient propofol to drive the spike back to baseline prevents incipient arousal. Preventing arousal prevents nociception[19].
After tumescent anesthesia injections, an opioid free, numb patient tends to remain immobile with liposuction. A not-in- frequent occurrence may be patient movement during propofol sedation. How can movement generated from the cortex, suggesting inadequate hypnosis (with possible awareness) be differentiated from movement generated from sub-cortical or spinal cord regions suggesting inadequate analgesia (no awareness)? The surgeon assumes epinephrine-induced vasoconstriction equals adequate analgesia and demands deeper sedation to terminate the movement. Vasoconstriction only guarantees adequate epinephrine effect. The anesthesiologist responds to the surgeon’s demand by asking for more local analgesia. Resolving this dilemma may be very much to the patient’s benefit by avoiding unnecessarily excessive, unneeded medications.
Patient movement without EMG spike defines sub-cortical generated movement origin without awareness risk. Patient movement without EMG spike also defines inadequate analgesia. Re-injection of the immediate area of stimulation resolves 98-99% of the sub-cortical generated patient movement[7]. Re-injection of the entire surgical filed is unnecessary. Patient movement with EMG spike defines cortical origin movement and requires additional hypnosis with sufficient propofol to bring the EMG spike back to baseline[7].
Morbidly obese patients sometimes seek liposuction. Fig. 5 The airway and distribution volume for propofol are unique considerations in the morbidly obese. The obese patient trends to have a thicker tongue and neck compared to non-obese patients. The morbidly obese tend to have a greater incidence of obstructive sleep apnea (OSA). In addition to no PONV and no antiemetics, opioid avoidance minimizes propofol respiratory depression. Morbidly obese patients also have a greater blood volume of distribution than the typical 70 kg patient making achieving a stable CNS propofol level more challenging. At 70 ml ˑ kg,-1 the 146 kg patient has a blood volume slightly more than 10 liters. A propofol bolus induction is the invitation to the difficult airway as well as a greater challenge creating a stable CNS propofol level with redistribution occurs.
This patient had 1,500 ccs liposuction in each of her upper arms. Approximately 2,000 ccs tumescent fluid was injected in each upper arm. Brain size does not vary proportionately with body weight. A 146 kg patient does not have a correspondingly twice the brain size of a 73 kg one. Ketamine 50 mg IV after propofol induction provided immobility for the tumescent injections.
Airway management for this patient’s induction was incremental and progressive. Initially her chin was extended, and her head was initially rotated to the right side, the so-called rhytidectomy or facelift position. When that was insufficient to maintain her airway, a 1,000 cc unheated IV bag was inserted under her shoulders to increase the force of extension on the genioglossus muscle. After those two initial non-invasive maneuvers did not maintain her airway, a nasal airway was inserted. This was sufficient to maintain this patient’s airway and the fourth (final) maneuver of LMA was not needed. Over 26 years, in none of more than 6,000 opioid free propofol, then ketamine patients was endotracheal intubation required. Oxygen 1 L. min-1 was also administered in this case. She emerged minutes after the discontinuation of the propofol infusion without either pain or PONV.

Figure 5. Morbidly obese 146 kg patient.
-
Conclusion
Friedberg’s Triad for opioid free anesthesia is a simple, minimally invasive paradigm useful even for morbidly obese patients. Processed EEG monitoring was especially useful with patients having greater than 5 liters blood volume to assure propofol levels remained in the hypnotic (60 < BIS < 75 with baseline EMG) zone throughout the surgery. Ketamine associated hallucinations were avoided. Immobility from the pain of tumescent anesthesia injections was eliminated with a unit ketamine does of 50 mg independent of weight or age.
-
References
1. Friedberg BL. Can Friedberg’s Triad Solve Persistent Anesthesia Problems? Over-Medication, Pain Management, Postoperative Nausea and Vomiting. Plast Reconstr Surg Glob Open. 2017 Oct;5(10):e1527–734. https://doi.org/10.1097/GOX.0000000000001527 PMID:29184740
2. Mulier J. Opioid free general anesthesia: A paradigm shift? Rev Esp Anestesiol Reanim. 2017 Oct;64(8):427–30. https://doi.org/10.1016/j.redar.2017.03.004 PMID:28431750
3. Hakim KY, Wahba WZ. Opioid-Free Total Intravenous Anesthesia Improves Postoperative Quality of Recovery after Ambulatory Gynecologic Laparoscopy. Anesth Essays Res. 2019;13(2):199–203. https://doi.org/10.4103/aer.AER_74_19 PMID:31198230
4. Friedberg BL. Minimally invasive anesthesia for minimally invasive surgery. Outpt Surg Mag Herrin Publishing Partners LP, Paoli, PA. 2004;2:57. https://lnkd.in/gASEJXKK
5. Friedberg BL. Hypnotic doses of propofol block ketamine-induced hallucinations. Plast Reconstr Surg. 1993 Jan;91(1):196–7. https://doi.org/10.1097/00006534-199301000-00047 PMID:8416533
6. Friedberg BL. The difficult airway in office-based anesthesia. Plast Reconstr Surg. 2010 May;125(5):221e–2e. https://doi.org/10.1097/PRS.0b013e3181d51741 PMID:20440149
7. Friedberg BL. BIS monitoring transformed opioid-free propofol ketamine anesthesia from art to science for ambulatory cosmetic surgery. Aesthetic Plast Surg. 2020 Dec;44(6):2308–11. https://doi.org/10.1007/s00266-020-01987-6 PMID:33037472
8. Friedberg BL. Propofol ketamine with bispectral (BIS) index monitoring chapter. In: Friedberg BL, editor. Anesthesia in Cosmetic Surgery. New York: Cambridge University Press; 2007. pp. 1–13. https://doi.org/10.1017/CBO9780511547218.004.
9. Friedberg BL. Ketamine associated laryngospasm during processed EEG monitored propofol sedation. Transl Perioper Pain Med. 2020;7:291–3.
10. Macario A, Weinger M, Truong P, Lee M. Which clinical anesthesia outcomes are both common and important to avoid? The perspective of a panel of expert anesthesiologists. Anesth Analg. 1999 May;88(5):1085–91. PMID:10320175
11. Macario A, Weinger M, Carney S, Kim A. Which clinical anesthesia outcomes are important to avoid? The perspective of patients. Anesth Analg. 1999 Sep;89(3):652–8. https://doi.org/10.1213/00000539-199909000-00022 PMID:10475299
12. Friedberg BL. Propofol-ketamine technique: dissociative anesthesia for office surgery (a 5-year review of 1264 cases). Aesthetic Plast Surg. 1999;23(1):70–5. https://doi.org/10.1007/s002669900245 PMID:10022941
13. Friedberg BL. Cosmetic surgery: postoperative pain and PONV – dissociative anesthesia reconsidered. Plast Reconstr Surg. 2010;125:184e–5e. https://doi.org/10.1097/PRS.0b013e3181d45e40 PMID:20335857
14. Apfel CC. Postoperative Nausea and Vomiting #97/112 ch. Miller’s Anesthesia. 8th ed. Philadelphia (PA): Elsevier; 2015.
15. Klein JA. Tumescent technique for regional anesthesia permits lidocaine doses of 35 mg/kg for liposuction. J Dermatol Surg Oncol. 1990 Mar;16(3):248–63. https://doi.org/10.1111/j.1524-4725.1990.tb03961.x PMID:2179348
16. Klein JA, Jeske DR. Estimated Maximal Safe Dosages of Tumescent Lidocaine. Anesth Analg. 2016 May;122(5):1350–9. https://doi.org/10.1213/ANE.0000000000001119 PMID:26895001
17. Ostad A, Kageyama N, Moy RL. Tumescent anesthesia with a lidocaine dose of 55 mg/kg is safe for liposuction. Dermatol Surg. 1996 Nov;22(11):921–7. https://doi.org/10.1111/j.1524-4725.1996.tb00634.x PMID:9063507
18. Practice Advisory for Intraoperative Awareness and Brain Function Monitoring Anesthesiol 2006;104:847–64
19. Friedberg BL, Sigl JC. Clonidine premedication decreases propofol consumption during bispectral index (BIS) monitored propofol-ketamine technique for office-based surgery. Dermatol Surg. 2000 Sep;26(9):848–52. https://doi.org/10.1046/j.1524-4725.2000.00074.x PMID:10971558

 ORCID
ORCID

