Nancy Raouf Wagid Nawar M.B.B.CH., M.Sc.1 , Gehan Fouad Kamel Youssef2, Azza Atef Abd El-Alem Ahmed2, Osama Ramzy Youssef Abd El-Malek2, Ramy Ahmed Mahrose Ahmed3
Recibido: 03-07-2024
Aceptado: 02-09-2024
©2024 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 53 Núm. 6 pp. 605-613|https://doi.org/10.25237/revchilanestv53n6-09
PDF|ePub|RIS
Comparación de eficacia analgésica entre bloqueos pectoral mayor tipo II, erector de la espina y paravertebral
Abstract
Introduction: Breast cancer surgeries are common surgical procedures, particularly in middle-aged women. Ultrasound guided chest wall blocks have become popular for regional analgesia in breast surgery. Objectives: Comparison between the analgesic efficacy of Pectoralis Major II (PECS II), paravertebral (PVB) and erector spinae (ESPB) blocks in analgesia postoperatively in modified radical mastectomy (MRM). Material and Methods: This prospective randomized comparative clinical study was conducted on 150 female patients, 30-70 years-old, ASA I-II, for unilateral elective MRM with axillary clearance, randomized into 3 groups each received ultrasound guided PECS II, or ESPB or PVB then followed up for 24 hours postoperatively. The primary outcome compared between the postoperative analgesic effect of PECS II with ESPB with PVB by Visual Analogue Score (VAS). The secondary outcomes compared total morphine consumption 24 hours postoperatively, sensory blockage and duration of block. Results: VAS in PECS II had lower score 24 hours postoperative. According to morphine consumption, PECS II had less morphine consumption than the other two groups. ESPB had prolonged duration of block followed by PVB with slight difference to PECS II. Regarding to axillary clearance, PECS II was the best in particular to coverage of axillary clearance. Conclusion: PECS II block is better than ESP block and PVB regarding analgesia starting from 0.5 hr. till 24 h postoperatively, with less narcotic consumption and better sensory blockage.
Resumen
Introducción: Las cirugías de cáncer de mama son procedimientos quirúrgicos comunes, particularmente en mujeres de mediana edad. Los bloqueos de la pared torácica guiados por ultrasonido se han vuelto populares para la analgesia regional en cirugía mamaria. Objetivos: Comparación entre la eficacia analgésica de Pectoralis Bloqueos mayor II (PECS II), paravertebral (PVB) y erector de la columna (ESPB) en analgesia posoperatoria en mastectomía radical modificada (MRM). Material y Métodos: Este estudio clínico comparativo, prospectivo, aleatorizado en 150 pacientes mujeres, de 30 a 70 años, ASA I II, para MRM electiva unilateral con vaciamiento axilar, aleatorizados en 3 grupos, cada uno de los cuales recibió PECS II guiado por ultrasonido, o ESPB o PVB. Se realizo seguimiento luego seguimiento durante 24 h posoperatorias. El resultado primario comparado entre el efecto analgésico posoperatorio de PECS II con ESPB con PVB mediante puntuación visual analógica (VAS). Los resultados secundarios compararon el consumo total de morfina 24 h después de la operación, el bloqueo sensitivo bloqueo y duración del bloqueo. Resultados: El EVA en PECS II tuvo menor puntuación a las 24 h del posoperatorio. Según el consumo de morfina, PECS II tenía menos consumo de morfina que los otros dos grupos. ESPB tuvo una duración prolongada del bloqueo seguido de PVB con ligera diferencia al PECS II. En cuanto al aclaramiento axilar, PECS II fue el mejor en particular en cuanto a la cobertura del vaciamiento axilar. Conclusión: el bloque PECS II es mejor que el bloqueo ESP y PVB en cuanto a analgesia a partir de 0,5 h hasta las 24 h del postoperatorio, con menor consumo de narcóticos y mejor bloqueo sensorial.
-
Introduction
MRM has always showed remarkable postoperative pain [1].
The thoracic region surgeries are associated with low tolerance acute pain and cause pathophysiological changes leading to chronic pain. So many regional blocks were developed for postoperative analgesia for MRM[2].
The PVNB is one of the analgesic methods capable of analgesia and reduction of opioid consumption in both the acute and late postoperative pain in breast surgeries[3].
One of the recent blocks used for analgesia in MRM is ESP. The technique of ESPB is by on the injection of local anesthetic in plane between the transverse process and erector spinae muscle[4].
In 2012, Pectoralis Major I,II blocks were firstly explained. The lateral and medial pectoral nerves are blocked in PECS I, while PECS II targets the intercostal nerve’s lateral branch. PECS II is useful in blocking intercostobrachial and long thoracic nerves and targets the axilla and intercostal nerves incision[5].
This study is designed to compare the analgesic efficacy of PECS II, PVB and ESPB in postoperative analgesia in MRM.
-
Material and Methods
This randomized prospective comparative clinical study was performed in Ain Shams University Hospitals in Breast surgeries unit and was granted the approval of the institutional ethics committee; Research Ethics Committee (REC) with identification No. FMASU MD 230/2021. The Declaration of Helsinki principles were followed in this study and had the approval of Pan African Clinical Trial Registry with identification No. PACTR 202309889843982 and written informed consent.
The study was performed on 150 female patients, 30-70 years old, with body mass index (BMI) < 35 kg.m-2 and the American Society of Anaesthesiologists’ (ASA) I-II enrolled for elective MRM and axillary clearance from 3 Nov 2021 to 2 Nov 2022.
Exclusion criteria included: BMI more than 35 kg.m-2, patients on anticoagulants or antiplatelets or with bleeding diathesis, significant psychiatric or mental disorders, known allergic reactions to local anaesthesia, neuropathy or neurological
deficits and infection close to block site and most important patient refusal,
Patients were divided randomly into 3 equal groups for each group receives one block after completion of surgery by ultrasound (US) guidance by injection of 20 ml bupivacaine 0.25%.
Group (A): received PECS II, Group (B): received ESPB, and Group (C): received PVB.
Each patient was assessed in the pre-operative visit including clinical examination and routine investigations.
On arrival, an Intravenous (IV) access was inserted, and standard monitors were connected; non-invasive electrocardiogram (ECG), arterial blood pressure (NIBP), and pulse oximetry (SpO2). Midazolam (0.035-0.05) mg/kg IV was injected for each patient for anxiolysis.
General anaesthesia was induced by propofol (1.5-2 mg/kg) IV, fentanyl (1 mic/kg) IV, and atracurium (0.5 mg/kg) IV for tracheal intubation. The maintenance of general anaesthesia was by Isoflurane (1.2-2%), also intravenous fluids were introduced. After completion of surgery, ultrasound guided block by a high- frequency transducer linear probe (6-12 MHz) connected to a Sonosite Fujifilm US machine and protected by sterile cover by a 100 mm, 22 gauge needle with a blunt end was used (B. Braun Medical Inc., Bethlehem, PA).
All patients were sequentially numbered opaque sealed envelope technique (SNOSE} divided using a computer-generated lists into 3 groups.
All groups had skin preparation by 10% povidone iodine.
-
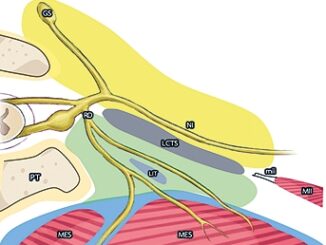
A) PECS II technique
The patient was supine then the coracoid process was identified in the sagittal paramedian plane. Then rotates the lower border of the transducer and slides laterally to introduce the needle an in-plane approach at 1-3 cm depth also the thoracoacromial artery can be identified. The success of block was confirmed by widening of the space between the pectoralis minor and pectoralis major after injection of 10 ml of LA. Then the second rib, axillary vein and artery were identified by placing the transducer at the midclavicular line and directing inferolaterally. By placing the transducer laterally, the practitioner can identify the serratus anterior, and pectoralis minor muscle easily. The third and fourth rib can be visualized by sliding the transducer laterally. LA is deposited the interfascial plane between the ser-
ratus anterior and pectoralis minor at 3-6 cm depth (Figure 1-a).
-
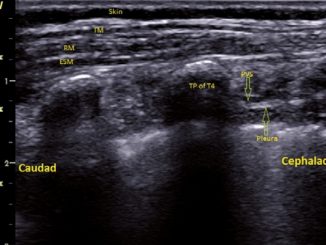
B) ESP Block technique
The patient was positioned the side to be blocked upwards after placing in lateral position. The block was performed at fourth thoracic vertebrae T4. The practitioner placed the probe 2-3 cm lateral to the spine sagittaly. After visualizing the Erector Spinae muscle (ESM) and the transverse processes the needle was inserted in an in plane approach. The LA is injected deep to ESM just superficial to T4 transverse process. LA spread was seen in both cranial and caudal directions (Figure 1-b).
-
C) PVB technique
The patient was also placed in lateral position similar to ESPB and the side to be blocked upwards, the block was performed at T4.
The practitioner placed the US probe about 5 cm lateral to the midline at T4 to identify the ribs and the pleura. The lung tissue appeared to be jet black deep to pleura.
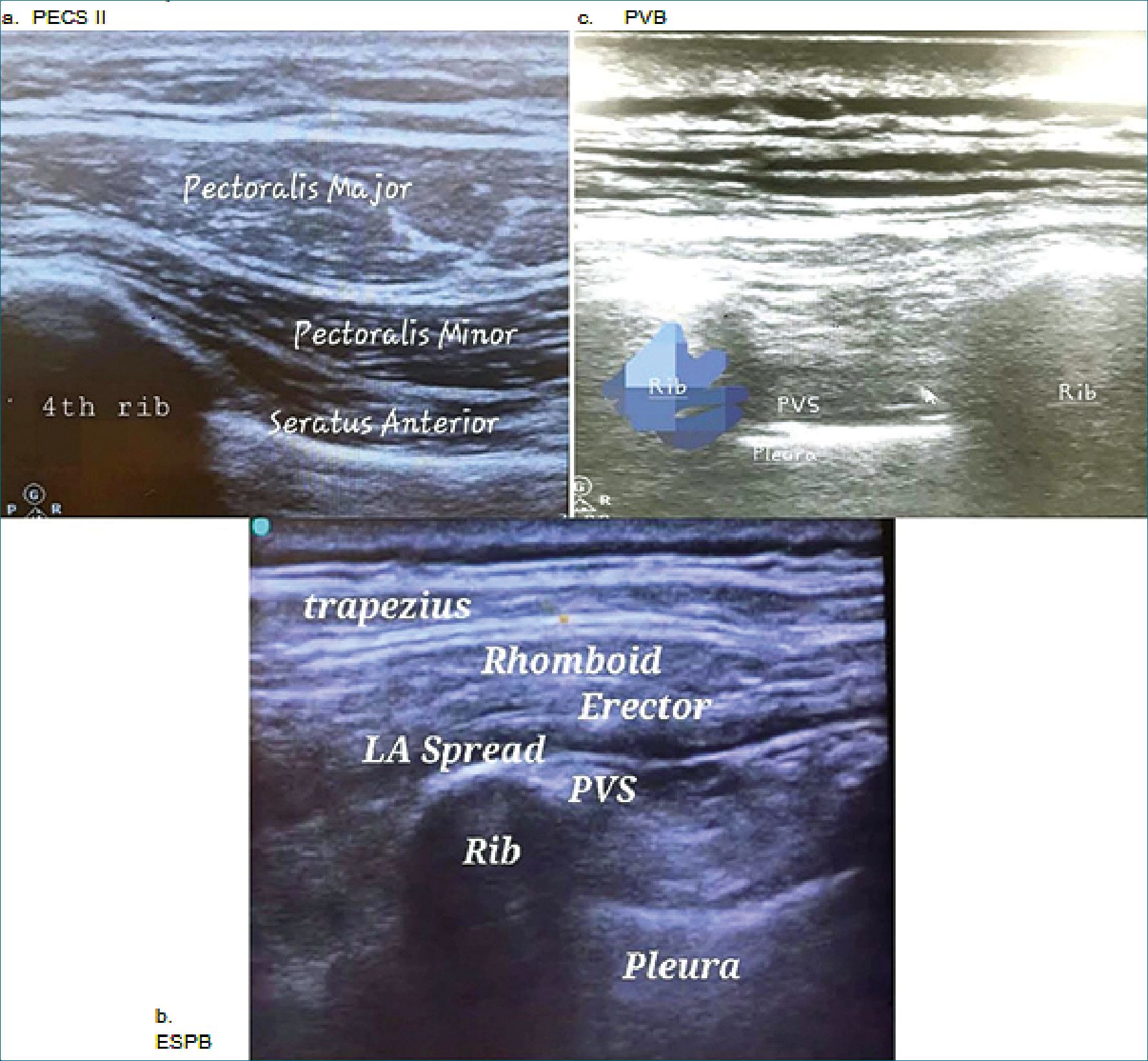
Figure 1. US view a: PECS II view; b: ESPB view; c: PVB view PVS = Paravertebral space.
The transition of ribs to transverse processes were visualized by sliding the probe.
To identify the paravertebral space the transducer was placed cranially, then needle was introduced to inject LA in an in-plane approach. The success of the block is confirmed by widening of PVS and depression of pleura (Figure 1-c).
After performing the block, Atropine 0.01 mg/kg and Neostigmine 0.05 mg/kg were injected for reversal of the neuromuscular blockade, and extubation was performed after fulfilling extubation criteria, then patients were referred to the post anaesthesia care unit (PACU) and standard monitoring were connected to the patient.
The pain assessment after complete recovery was accessed by visual analogue scale (VAS). The scale is a line having two ends ,the left end (0 cm) indicates “no pain”, and the right end indicates (10 cm) “worst pain”. Patients would choose the score according to symptoms then recorded along the length of a 10-cm line the point indicating pain severity.
The primary outcome is comparing VAS scores between the three groups, while the secondary outcome was to compare between total opioid consumption, sensory blockage and duration of analgesia.
VAS score was recorded in the PACU at 0.5 h, 2 h, 4 h, 8 h, 12 h, and 24 h postoperatively. Whenever VAS score > 3, Morphine 2 mg IV was introduced until VAS score = 3, with maximum dose 10 mg in PACU, while in the surgical ward, 3 mg Morphine IV was given within 2 hours whenever the VAS score was more than 3, until VAS was 3. In three groups, total postoperative opioid consumption was recorded in the first 24 h. Also, sensory blockage was accessed by cold object to identify the dermatomal blockage 2 h postoperative. Also, block duration was recorded at 24 h postoperative.
-
Sample size
Sample size was calculated by G power program, setting power at 80%, medium effect size (0.5), a-error = 0.05. It is estimated that the sample size of 50 patients in each group which can detect a statistically significant difference between each group regarding VAS pain score (Visual Analogue Score) and Morphine consumption postoperative for 24 h corresponding to a medium effect size of 0.5[6].
-
Statistical analysis
All data were tabulated, coded and analyzed by IBM SPSS statistics (Statistical Package for Social Sciences) software version 28.0, IBM Corp., Chicago, USA, 2021. Kolmogorov- Smirnov test was used to test quantitative data, then described as mean ± SD (standard deviation) as well as maximum and minimum of the range, and then they were compared using ANOVA test. Qualitative data was expressed as percentage and number and was compared using Fisher’s Exact test and Chi square test. Rate of first morphine consumption was compared by Log rank test. Bonferroni test used for post hoc comparisons. p-value < 0.050 was significant, any other was non-significant.
Table 1. Comparison between the three studied groups regarding their demographic data
| Variables | PECS II (Total = 50) | ESB (Total = 50) | PVB (Total = 50) | p-value | |
| Age (years) | Mean±SD | 52.6 ± 9.3 | 50.9 ± 7.9 | 52.1 ± 8.4 | A0.597 |
| Range | 34.0 – 69.0 | 37.0 – 69.0 | 36.0 – 69.0 | ||
| BMI (kg/m2) | Mean±SD | 29.8 ± 1.7 | 29.6 ± 1.9 | 29.5 ± 1.8 | A0.770 |
| Range | 26.1 – 32.9 | 24.1 – 33.1 | 24.1 – 33.0 | ||
| ASA (n, %) | I | 9 (18.0%) | 8 (16.0%) | 8 (16.0%) | #0.953 |
| II | 41 (82.0%) | 42 (84.0%) | 42 (84.0%) | ||
| Operation duration | Mean±SD | 142.5 ± 13.4 | 141.0 ± 13.4 | 141.3 ± 12.6 | A0.839 |
| (min) | Range | 122.0 – 177.0 | 117.0 – 168.0 | 116.0 – 165.0 | |
BMI: Body Mass Index; ASA: American association of naethiologists; AANOVA test; #Chi square test.
-
Results
Table 2 showed that: T1 block was more frequent in PECS-II with no significant differences between ESP and PVB. T2 and 3 block was significantly least frequent in PVB with no significant
differences between PECS-II and ESP. The groups showed no significant differences regarding T4, 5 and 6 block. T7 block was least frequent in PECS-II with no significant differences between ESP and PVB. T8 block was most frequent in PVB with no significant differences between PECS-II and ESP (Table 1).
Regarding VAS score, pain at hours 0.5 and 12 as well as maximum pain score were highest in PVB, followed by ESB and lowest in PECS-II, the differences were significant between all the study groups. Pain at hours 2, 4 and 8 was significantly lowest in PECS-II with no significant differences between ESP and PVB. Pain at hour 24 was significantly highest in PVB with no significant differences between PECS-II and ESP.
Morphine consumption was absent in all the study groups in hours 0.5 and 2, then begain to rise at hour-4 in ESP and PVB groups, while in PECS-II group it began to rise at hour-12. Morphine consumption in hour 4 was significantly lowest in PECS-II with no significant differences between ESP and PVB. Morphine consumption in hour 8 was highest in ESB, followed by PVB and lowest in PECS-II, the differences were significant between all the study groups. Morphine consumption in hour was highest in PVB, followed by ESB and lowest in PECS-II, the differences were significant between all the study groups. Morphine consumption in hour-24 was non-significantly different between the study groups. Total 24-hour morphine consumption and morphine doses frequency were highest in PVB, followed by ESB and lowest in PECS-II, the differences were significant between all the study groups (Figure 3 and Table 3).
Number of blocked levels was significantly lowest in PVB, with no significant differences between PECS-II and ESB. Block duration was significantly shortest in PECS-II, with no significant differences between ESB and PVB (Figure 2-a) Time of first dose was significantly longest in PECS-II with no significant differences between PVB and ESPB (Figure 2-d).
-
Discussion
MRM is one of the most frequent procedures in breast surgery causing severe postoperative pain so pain management techniques, as patient-controlled analgesia and thoracic epidural are commonly used[7]. Opioids are commonly used for post-operative analgesia but are associated with suppression of cellular
Table 2. Block characteristics and (VAS-10) between the study groups
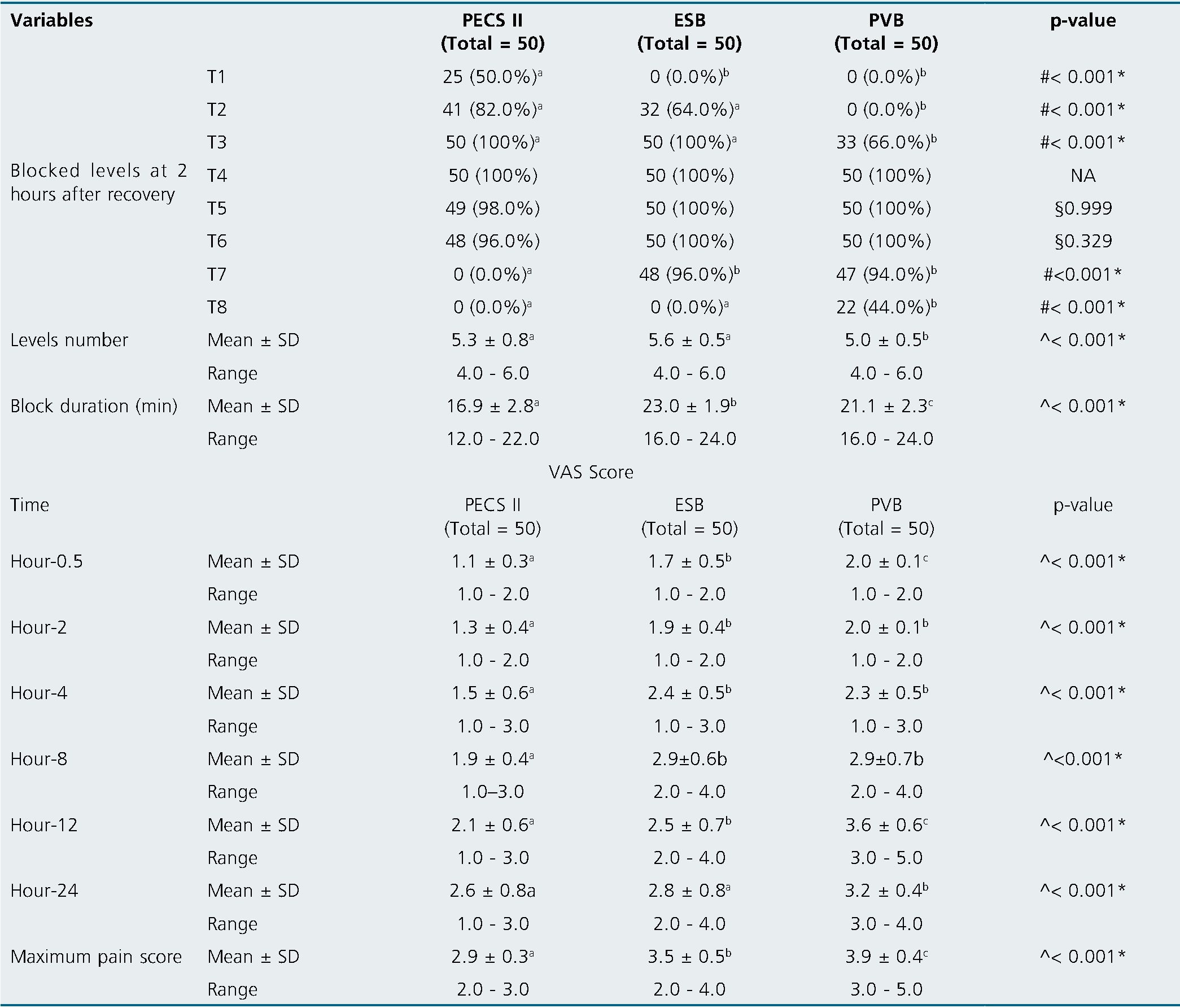
NA: Not applicable; AANOVA test; #Chi square test; §Fisher’s Exact test; *Significant; Homogenous groups had the same symbol “a,b,c” based on post hoc Bonferroni test.
immunity, higher cancer recurrence and more risk of nausea and vomiting postoperatively[8].
By the rise of the peripheral and truncal blocks, new techniques of thoracic wall blocks are introduced so ultrasound improves the efficacy and safety. Thoracic epidural and PVB are still considered the corner stone of regional techniques.Unfortunatly,they are accompanied by complications for example vascular puncture or nerve injury or most serious tension pneumothorax[9].
In 2012, Blanco et al.[10], discussed the PECS I and PECS II for breast surgeries and had excellent postoperative analgesia. This study revealed that PECS II was given to MRM patients and had better analgesia and less postoperative morphine consumption 24 hours postoperative.
In this study, results were like Altiparmak and colleagues [11] who compared between PECS block with ESP in a study that included 40 patients undergoing MRM and found superiority of PECS II than ESPB and concluded that better analgesia seen in PECS block because of the blockade of thoracodorsal, long thoracic, medial and lateral pectoral nerves.
In favour to our results, Bakeer and Abdallah[12] concluded that after conducting PECS II and Erector Spinae on 60 females showing superiority of PECS II in reduced VAS score over ESPB as mean of VAS score after 2 hours for PECS II group was 1-3 and in this study the range was 1-2, while in ESPB, 1-4 but in this study, 1-2 after 12 hours in PECS II group showed 0-3 in this study 1-3 while in ESPB 1-4 and this study had a range 2-4.
Axillary pain were observed to be lower in PECS II up to 24 hours postoperative. The explanation for coverage of axillary pain is due to the spread of LA to an axillary port assuring the blockage of the intercostobrachial and medial brachial cutaneous
nerves[13]. This explanation was useful in understanding the results of this study as 50% of patients whom received PECS II had T1 and T2 blockage.
According to Sinha and colleagues [14] discussed the total consumption of post operative morphine after conducting on 64 female patients undergoing MRM found total morphine consumption in PECS II block 4.4 ± 0.94 and ESPB 6.5 ± 1.35.
Bakshi et al.[15], have notified the difficulty of the surgical
technique due to fluid filling the interfascial plane after PECS II block. In this study this problem is overcomed by performing the block postoperatively.
ESP block for thoracic surgeries was introduced by Forero and his colleagues [16] in a case report that had failed epidural procedure in 2016.
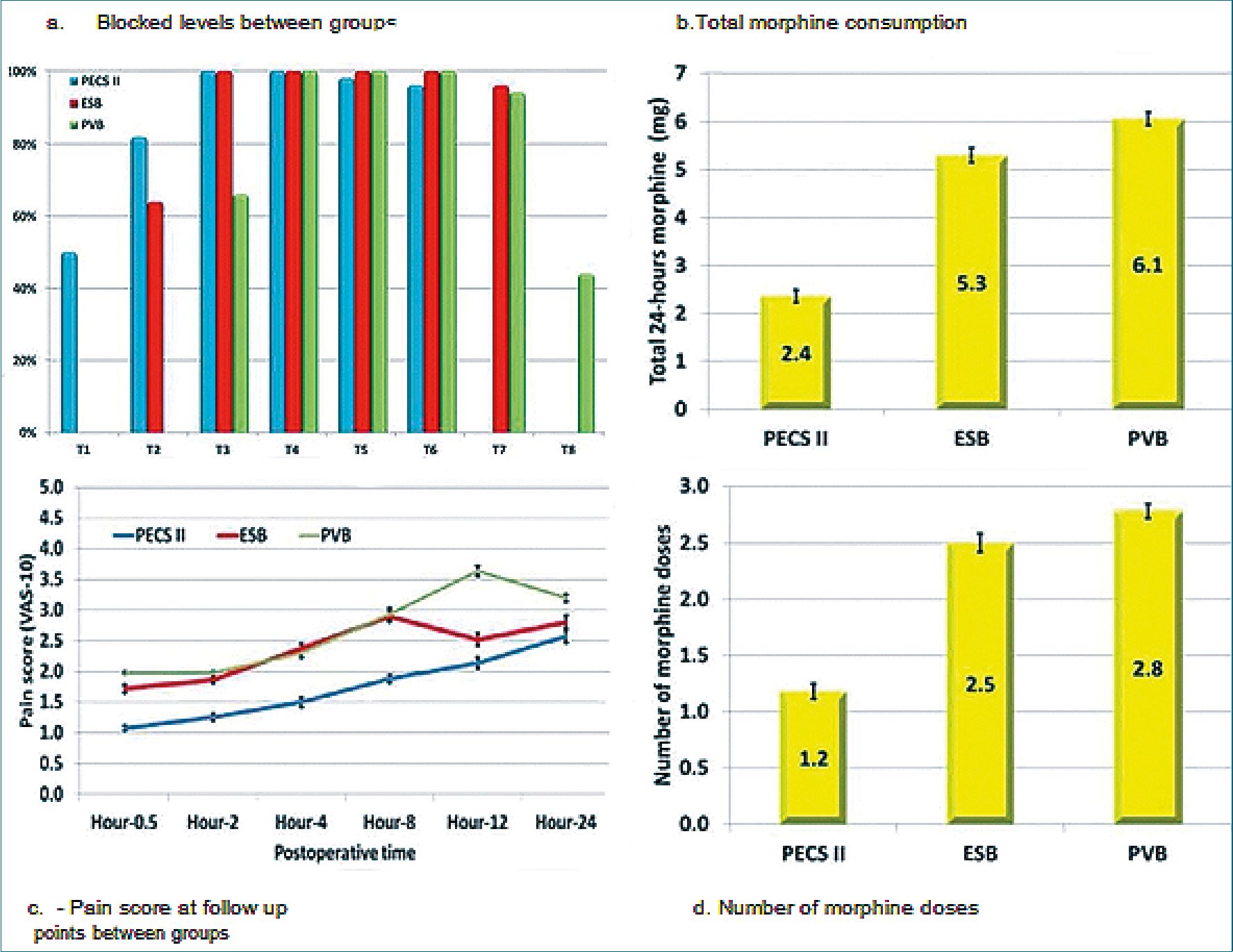
Figure 2. a: Blocked levels between groups; b: Total 24-hours morphine consumption between groups; c: Pain score at follow up points between groups) (d- Number of morphine doses between groups).
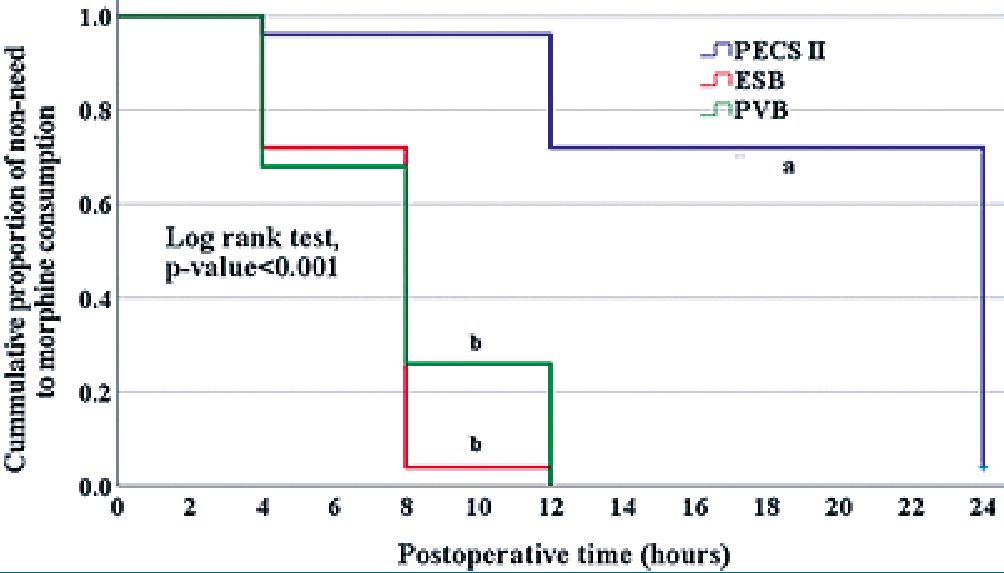
Figure 3. Kaplan-Meier curve for rate of first morphine consumption between the groups. Homogenous groups had the same symbol “a,b” based on post hoc Bonferroni test.
In thoracic surgeries ,It is usually performed at T4 allowing LA spread craniocaudally and anteriorly in costotransverse foramina reaching PVS[17]. Although there are several studies showed that ESP block is a better option than PVB due to safety and better spread of LA craniocaudally. Veiga et al.[18], notified that the radiocontrast dye used in cadaveric models might not reach the paravertebral space anteriorly to reach the origins of the dorsal and ventral thoracic nerves[19]. This limitation explains our findings that ESP is accompanied by more postsurgical opioid dose, and less pain control.
Consistent to this study also Oza and collegues[20] injected 25 ml 0.25% bupvicaine for ESPB for females undergoing MRM, duration of block was in range of 18.23 ± 1.67 hours postoperative which approximately like this study.
In a recent study Mohsin and collegues[21] conducted on 90 patients comparing between ESPB, PECS and a control group showed like this study the total amount of analgesia consumption was higher in ESPB.
PVB blocks ipsilateral dermatomes without blockage of sympathetic chain on the other side. Also, PVB can’t block long thoracic, thoracodorsal , medial and lateral pectoral nerves so it doesn’t cover axillary clearance[22].
Many studies proved that PVB may lead to epidural blockage, total spinal anesthesia can also occur . Lonnqvist and colleagues[23] reported complications like vascular puncture,hypotension and pneumothorax (0.5%) in 367 patients.
Gurkan and colleagues[24], used ESPB versus PVB in postoperative analgesia in MRM which found equal results that during 24 h postoperative the mean of morphine was 5.6 ± 3.43 mg in ESPB, and in PVB 5.64 ± 4.15 mg.
According to this study there was slight increase in analgesic consumption in PVB but very close to ESPB results in coverage and duration of the block.
This study showed lower VAS score in first ^,2,4,8,12 hours up to 24 hours more in PECS group followed by ESPB and slight difference between PVB and ESPB also the results showed the need for analgesia in PECS II was (n = 48 or 96%) in ESPB and PVB were n = 50 or 100% , the need for first dose was approximately equal in ESPB and PVB with range 4 h to 12 h.
In support to this study, Elewa and collegues[25], designed a study on 90 patients undergoing MRM to comparing ESPB, PVB and control group which showed lower VAS score in ESPB. In ESPB ,VAS scores were lower than PVB and the control group during the first 24 h after the surery (p < 0.001). The duration of ESPB was longer than PVB as observed by the differences in the VAS score at 8 h (median in ESPB = 5 (4.75-6) versus PVB 6 (5 6.5),
p = 0.001 and 12 h (median ESPB = 5 (4-5) versus PVB 5 (4.5-6), p = 0.002
Siddeshwara and collegues[26] observed that PECS II was able to record longer block duration than PVB (PECS II = 474.1 ± 84.93 against PVB = 371.5 ± 51.53 min, P < 0.0001) and less total morphine consumption 24 h after surgery (PECSII = 11.25 ± 4.75 and PVB = 15.0 ± 4.86 mg, P = 0.018).
On the other hand, Martsiniv[27] concluded that there was no significant observed differences between PECS II and PVB groups in the postoperative pain scores during 24 h postoperative but the need to the first analgesia dose was longer in PECS II.
It was hypothesized in this study that the difference in the results of some studies can be due to some reasons. First, injecting different concentrations of the local anesthetics it definitely change the analgesic power of the block. Second, also on injecting large volume of LAs it affects the number of dermatomes covered. Third, the operator’s experience plays an important role in the quality of the block.
Regarding duration of block, ESPB was better than PVB then PECS with mean approximately of 17 hours postoperative especially that ESPB was injected by a high LA volume.
According to dermatomal coverage, PECS II block achieved better dermatomal coverage especially in axillary clearance as it blocked T2-T6 extending to midaxillary line which is optimum to breast surgery while ESPB and PVB block T4- T10 and partial coverage of axilla.
Table 3. Morphine consumption between the study groups
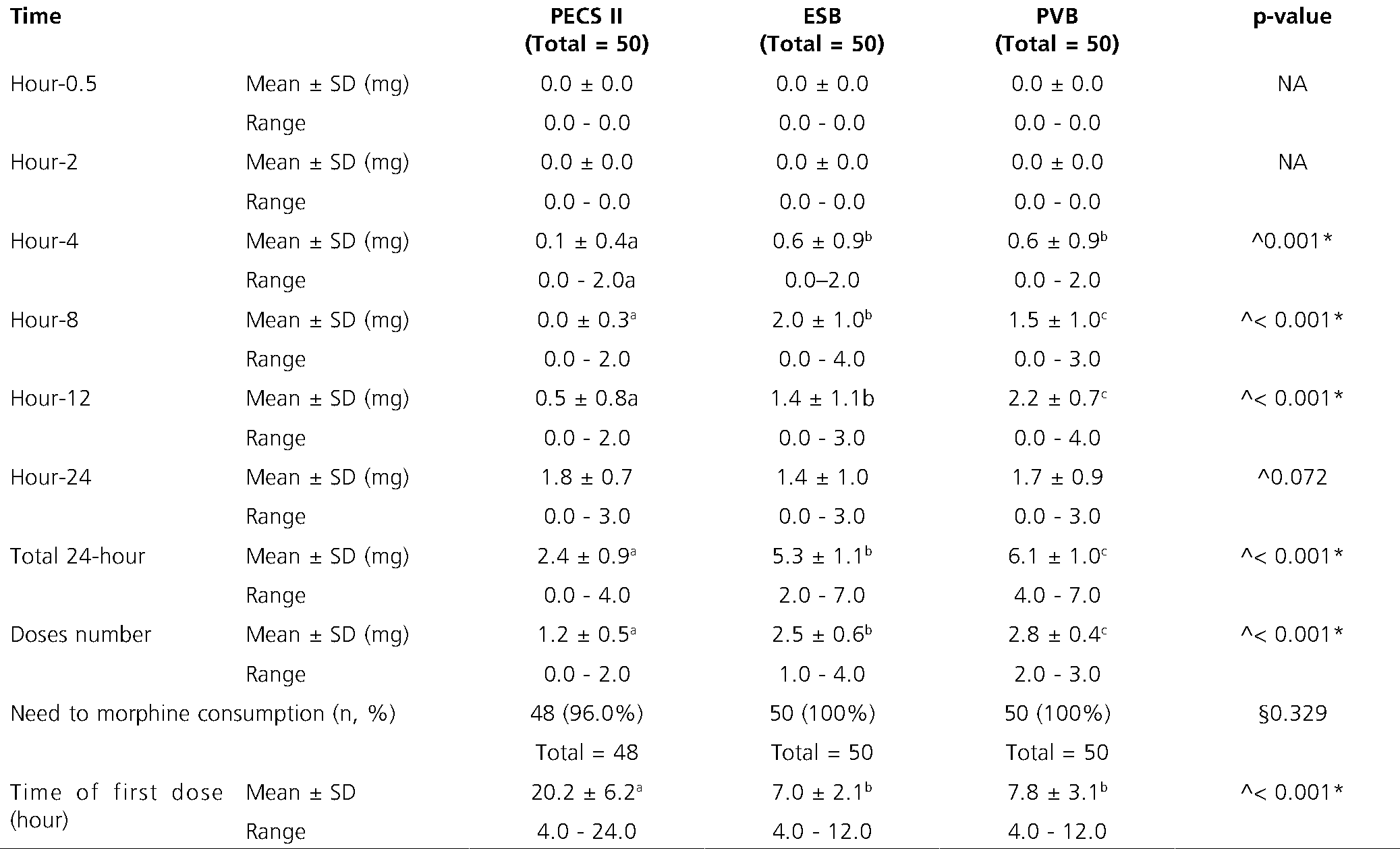
NA: Not applicable; AANOVA test; §Fisher’s Exact test; *Significant; Homogenous groups had the same symbol “a,b,c” based on post hoc Bonferroni test.
-
Limitations
First in PECS II block due to proximity to surgical site there was distortion in ultrasound view due to anatomical changes postoperative.
Variation in patient ages showed varibality in morphine consumption due to slower rate of metabolism.
-
Conclusion
PECS II block is better than ESP block and PVB regarding analgesia starting 24 h postoperatively, with less narcotic consumption and better sensory blockage.
Disclosure statement: No potential conflict of interest was reported by the authors.
Funding: No funding.
Reception data: 03 de julio de 2024 / Approvement: 02 de septiembre de 2024
-
References
1. Fecho K, Miller NR, Merritt SA, Klauber-Demore N, Hultman CS, Blau WS. Acute and persistent postoperative pain after breast surgery. Pain Med. 2009;10(4):708–15. https://doi.org/10.1111/j.1526-4637.2009.00611.x PMID:19453965
2. Shipton EA. The transition of acute postoperative pain to chronic pain: Part 1–Risk factors for the development of postoperative acute persistent pain. Trends Anaesth Crit Care. 2014;4(2-3):67–70. https://doi.org/10.1016/j.tacc.2014.04.001.
3. Kairaluoma PM, Bachmann MS, Korpinen AK, Rosenberg PH, Pere PJ. Single-injection paravertebral block before general anesthesia enhances analgesia after breast cancer surgery with and without associated lymph node biopsy. Anesth Analg. 2004 Dec;99(6):1837–43. https://doi.org/10.1213/01.ANE.0000136775.15566.87 PMID:15562083
4. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621–7. https://doi.org/10.1097/AAP.0000000000000451 PMID:27501016
5. Bashandy GM, Abbas DN. Pectoral nerves I and II blocks in multimodal analgesia for breast cancer surgery: a randomized clinical trial. Reg Anesth Pain Med. 2015;40(1):68–74. https://doi.org/10.1097/AAP.0000000000000163 PMID:25376971
6. El Ghamry MR, Amer AF. Role of erector spinae plane block versus paravertebral block in pain control after modified radical mastectomy. A prospective randomised trial. Indian J Anaesth. 2019 Dec;63(12):1008–14. https://doi.org/10.4103/ija.IJA_310_19 PMID:31879425
7. Yeh CC, Yu JC, Wu CT, Ho ST, Chang TM, Wong CS. Thoracic epidural anesthesia for pain relief and postoperation recovery with modified radical mastectomy. World J Surg. 1999 Mar;23(3):256–60. https://doi.org/10.1007/PL00013180 PMID:9933696
8. Kaye AD, Patel N, Bueno FR, Hymel B, Vadivelu N, Kodumudi G, et al. Effect of opiates, anesthetic techniques, and other perioperative factors on surgical cancer patients. Ochsner J. 2014;14(2):216–28. PMID:24940132
9. Bashandy GM, Abbas DN. Pectoral nerves I and II blocks in multimodal analgesia for breast cancer surgery: a randomized clinical trial. Reg Anesth Pain Med. 2015;40(1):68–74. https://doi.org/10.1097/AAP.0000000000000163 PMID:25376971
10. Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of Pecs II (modified Pecs I): a novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012 Nov;59(9):470–5. https://doi.org/10.1016/j.redar.2012.07.003 PMID:22939099
11. Altıparmak B, Korkmaz Toker M, Uysal Aİ, Turan M, Gümüş Demirbilek S. Comparison of the effects of modified pectoral nerve block and erector spinae plane block on postoperative opioid consumption and pain scores of patients after radical mastectomy surgery: A prospective, randomized, controlled trial. J Clin Anesth. 2019 May;54:61–5. https://doi.org/10.1016/j.jclinane.2018.10.040 PMID:30396100
12. Bakeer A, Abdallah NM. Erector spinae plane block versus pecs block type II for breast surgery: a randomized controlled trial. Anesth Pain Med. 2022 Apr;12(2):e122917. https://doi.org/10.5812/aapm-122917 PMID:35991781
13. Torre PA, Jones JW Jr, Álvarez SL, Garcia PD, Miguel FJ, Rubio EM, et al. [Axillary local anesthetic spread after the thoracic interfacial ultrasound block – a cadaveric and radiological evaluation]. Rev Bras Anestesiol. 2017;67(6):555–64. https://doi.org/10.1016/j.bjan.2016.10.009 PMID:28867151
14. Sinha C, Kumar A, Kumar A, Prasad C, Singh PK, Priya D. Pectoral nerve versus erector spinae block for breast surgeries: A randomised controlled trial. Indian J Anaesth. 2019 Aug;63(8):617–22. https://doi.org/10.4103/ija.IJA_163_19 PMID:31462806
15. Bakshi SG, Karan N, Parmar V. Pectoralis block for breast surgery: A surgical concern? Indian J Anaesth. 2017 Oct;61(10):851–2. https://doi.org/10.4103/ija.IJA_455_17 PMID:29242663
16. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621–7. https://doi.org/10.1097/AAP.0000000000000451 PMID:27501016
17. Altıparmak B, Korkmaz Toker M, Uysal Aİ, Turan M, Gümüş Demirbilek S. Comparison of the effects of modified pectoral nerve block and erector spinae plane block on postoperative opioid consumption and pain scores of patients after radical mastectomy surgery: A prospective, randomized, controlled trial. J Clin Anesth. 2019 May;54:61–5. https://doi.org/10.1016/j.jclinane.2018.10.040 PMID:30396100
18. Veiga M, Costa D, Brazão I. Erector spinae plane block for radical mastectomy: A new indication? Rev Esp Anestesiol Reanim (Engl Ed). 2018 Feb;65(2):112–5. https://doi.org/10.1016/j.redare.2017.12.001 PMID:29102405
19. Ivanusic J, Konishi Y, Barrington MJ. A Cadaveric Study Investigating the Mechanism of Action of Erector Spinae Blockade. Reg Anesth Pain Med. 2018 Aug;43(6):567–71. https://doi.org/10.1097/AAP.0000000000000789 PMID:29746445
20. Oza V, Vadgama PD, Parmar VS, Rawal KK. A study of efficacy of iitv-guided erector spinae plane (ESP) block as novel multimodal analgesia technique for postoperative analgesia in modified radical mastectomy (MRM). Int J Acad Med Pharm. 2024;6(1):991–5.
21. Mohsin MH, Verma R, Hemlata, Singh D, Singh S, Singh K. Effect of Erector Spinae Block and Pectoralis Block on Quality of Recovery and Analgesia After Modified Radical Mastectomy: A randomised controlled study. Sultan Qaboos Univ Med J. 2023 May;23(2):220–6. PMID:37377822
22. Terheggen MA, Wille F, Borel Rinkes IH, Ionescu TI, Knape JT. Paravertebral blockade for minor breast surgery. Anesth Analg. 2002 Feb;94(2):355–9. https://doi.org/10.1213/00000539-200202000-00023 PMID:11812698
23. Lönnqvist PA, MacKenzie J, Soni AK, Conacher ID. Paravertebral blockade. Failure rate and complications. Anaesthesia. 1995 Sep;50(9):813–5. https://doi.org/10.1111/j.1365-2044.1995.tb06148.x PMID:7573876
24. Gürkan Y, Aksu C, Kuş A, Yörükoğlu UH. Erector spinae plane block and thoracic paravertebral block for breast surgery compared to IV-morphine: A randomized controlled trial. J Clin Anesth. 2020 Feb;59:84–8. https://doi.org/10.1016/j.jclinane.2019.06.036 PMID:31280100
25. Elewa AM, Faisal M, Sjöberg F, Abuelnaga ME. Comparison between erector spinae plane block and paravertebral block regarding postoperative analgesic consumption following breast surgery: a randomized controlled study. BMC Anesthesiol. 2022 Jun;22(1):189. https://doi.org/10.1186/s12871-022-01724-3 PMID:35717148
26. Siddeshwara A, Singariya G, Kamal M, Kumari K, Seervi S, Kumar R. Comparison of efficacy of ultrasound-guided pectoral nerve block versus thoracic paravertebral block using levobupivacaine and dexamethasone for postoperative analgesia after modified radical mastectomy: A randomized controlled trial. Saudi J Anaesth. 2019;13(4):325–31. https://doi.org/10.4103/sja.SJA_25_19 PMID:31572077
27. Martsiniv VV. Efficacy of the pectoral nerve block type II and paravertebral block for enhanced recovery after breast cancer surgery. Emerg Med. 2021;17(4):43–50. https://doi.org/10.22141/2224-0586.17.4.2021.237726.

 ORCID
ORCID