Raham Hasan Mostafa 1 , Amr Amin Rashwan 1 , Mohamed Mohamed AboKamar 1
Recibido: 27-08-2019
Aceptado: 12-10-2019
©2020 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 49 Núm. 4 pp. 560-563|https://doi.org/10.25237/revchilanestv49n04-12
PDF|ePub|RIS
Manejo anestésico para resección de insulinoma en un paciente portador de neuropatía desmielinizante crónica
Abstract
Chronic Inflammatory Demyelinating Polyneuropathy associated with hypoglycemia 2 to insulinoma is unusual, and to our knowledge, very few patients have been reported in literature. Despite varying presentations in these patients, the clinical characteristics are usually the same. The syndrome usually occurs after several episodes of protracted hypoglycemia. The neuropathy is nearly always symmetrical. We report anesthetic management for a young female patient presenting with CIDP & repeated hypoglycemic episodes during a 2-year period scheduled for insulinoma enucleation.
Resumen
La polineuropatía desmielinizante inflamatoria crónica asociada con hipoglicemia secundaria a insulinoma es inusual y, hasta donde sabemos, muy pocos pacientes han sido reportados en la literatura. A pesar de las diferentes presentaciones en estos pacientes, las características clínicas suelen ser las mismas. El síndrome generalmente ocurre después de varios episodios de hipoglicemia prolongada. La neuropatía es casi siempre simétrica. Presentamos el manejo anestésico para una paciente joven que se presenta con polineuropatía desmielinizante inflamatoria crónica y episodios repetidos de hipoglicemia durante un período de 2 años programado para la enucleación de insulinoma.
-
Introduction
Insulinoma is a rare endocrinal tumor that causes hypoglycemia, and surgical resection is its definite treatment. Chronic neuropsychiatric symptoms attributed to hypoglycemia are a well-known presentation of insulinoma. Peripheral neuropathy has been rarely reported in such patients. The first report of a case suggestive of peripheral neuropathy with an insulinoma was described by Silfverskiold in1946[1].
Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) is an acquired inflammatory disorder of unknown etiology affecting the peripheral nervous system (PNS). It is usually with motor involvement having symmetrical, proximal limb weakness. CIDP is not a common disease in our field with no enough guidelines for its specific anesthetic management. We report anesthetic management of a case of an insulinoma enucleation associated with CIPD.
-
Case presentation
A 33 year old female was scheduled for enucleation of insulinoma. The history started 2 years ago with recurrent fits and behavioral changes. She was falsely diagnosed as epileptic. 8 months ago, a gradual onset of mild quardiparesis and ataxia occurred. She sought medical advice and was finally diagnosed as CIDP according to European Federation of Neurological Societies and the Peripheral Nerve Society (EFNS/PNS) criteria[2] following extensive workup and differential diagnosis. Other causes of acquired polyneuropathy were first excluded. During her admission for diagnosing her neurological manifestation, the recurrent hypoglycemic attacks alerted her physician for exclusion of insulinoma which was diagnosed by: whipple’s triad symptoms, 72-h fasting test and localized by 68Ga-DOTATATE PET/CT scan.
Preoperative assessment showed that the patient was fully conscious but with abnormal behavior & spontaneous screaming. Documentation of neurological deficit was done by a neurologist revealing dysarthria, bilateral upper limb (UL) ad bilateral lower limb (LL): ataxia, weakness & diminished deep tendon reflexes with no cranial nerve affection. She was fits free with no antiepileptic medications since she started continuous glucose infusion. During her hospital stay, blood glucose level was maintained at: 100-150 mg/dL by 100 mL/h Dextrose 10% infusion, with 2 hourly monitoring, and a bolus 100 mL of 25% during any hypoglycemic attacks. Besides, somatostatin treatment was started once the diagnosis of insulinoma was confirmed. All her preoperative laboratories were in normal range, 68Ga-DOTATATE PET/CT scan showed pedunculated soft tissue nodule measuring 1.2 x 1.1 cm with no lymph node or metastatic lesion detected.
In the operating room and just before induction of GA, her basal blood sugar was 200 mg/dL. Dextrose 10% infusion was continued at a basal rate of 100 ml/h. General anesthesia (GA) was started after application of full standard monitors. Preoxygenation was done for 3 min and rapid sequence induction of anesthesia was done using 1 µg/kg fentanyl, 1 mg/kg propofol, and rocuronium at a dose of 1 mg/kg then endotracheal intubation was done with an oral cuffed endotracheal tube while applying Sellick maneuver. Maintenance of anesthesia was done by Isoflurane 1-2 MAC and controlled mechanical ventilation.
Just after intubation, an arterial line was inserted for frequent blood sugar sampling and close hemodynamic observation. Blood sugar was checked once every 15 min until tumor was reached, and every 10 min once tumor manipulation was started. Blood sugar ranged between 150 to 250 mg/dL intraoperatively. The surgery was completed in 90 min. Sugammadex at a dose of 2 mg/kg was administered to reverse the effect of rocuronium. Patient was extubated successfully and was transferred fully conscious to the ICU. No major intraoperative events occurred.
Her postoperative course was uneventful, glucose infusion was stopped since ICU admission & she was discharged on second postoperative day to ward with no change in her preoperative neurological state.
-
Discussion
Insulinoma is a functioning endocrinal tumor arising from beta cells of the pancreas. They are rare tumors with an incidence of 1-4 per million per year with median age of presentation of 47 years, having a mild female predominance. Tumors are usually small and solitary at the time of diagnosis. They are usually benign and the history is often lengthy and mostly involves neuropsychiatric symptoms. Malignant insulinomas may be associated with Multiple Endocrine Neoplasia Type-1 (MEN -1) syndrome. Because of the bizarre nature of the presenting symptoms, many patients are usually misdiagnosed or have delayed diagnosis and are usually first presented to neurologists or psychiatrists[3].
Diagnosis of insulinoma is both: clinical, biochemical, with radiological localization of the tumor. Clinical diagnosis is based on Whipple’s Triad which includes repeated attacks of hypoglycemia, serum blood glucose levels < 50 mg/dl during that period and relief of symptoms with glucose administration. Biochemical diagnosis includes measuring: serum glucose, insulin, C-peptide, and proinsulin during the 72-h fasting test which is considered as a gold standard test. Localizing insulinomas are difficult with a failure rate of 10-27% as most tumors are often less than 2 cm and evenly present in any part of the pancreas. Non-invasive imaging procedures, such as computed tomography and magnetic resonance imaging, are usually used. 68Ga-DOTATATE/DOTATOC PET/CT has been described in the detection of insulinomas. It is a non-invasive imaging modality and can be used if all imaging studies were negative in a diagnosed patient[4].
Treatment includes medical and surgical management. Medical management includes dietary modification and pharmacological agents (Diazoxide & Somatostatin analogues). Surgical excision which is considered the definite treatment includes: enucleation or partial pancreatectomy[5 ].
CIDP is an acquired demyelinating disorder affecting the PNS which can be chronically progressive or follow a pattern of relapses and remissions. Although the etiology is unknown, one hypothesis is that this polyneuropathy is immunologically based and involves both humoral and cellular components of the immune system[6]. CIDP associated with islet cell tumors and hypoglycemia has been reported very rarely. Direct relationship to a single hypoglycemic insult is often absent. It is reasonable to hypothesize that the underlying mechanism involved in its pathogenesis is complex and multifactorial[7].
The diagnosis of CIDP according to European Federation of Neurological Societies and the Peripheral Nerve Society (EFNS/PNS) criteria is based on clinical history, physical examination, electrophysiology, and supporting laboratory tests[2]. Despite varying features in these patients, the clinical characteristics of this syndrome are remarkably similar. These consist of the development of symmetric sensorimotor neuropathy during a protracted course of recurrent hypoglycemia. Upper limb involvement is more frequent, accompanied by severe weakness & distal wasting. An overall decrease or absence of deep tendon reflexes is found in most cases. Painful distal parathesia is characteristic[7 ]. Different studies are required to confirm the diagnosis: electrophysiological examination and nerve biopsy. In terms of treatment, in severe or rapidly progressive cases, the treatment is based on IV immunoglobulins, plasmapheresis, corticosteroids or immunosuppressants[6].
-
Anesthetic implications
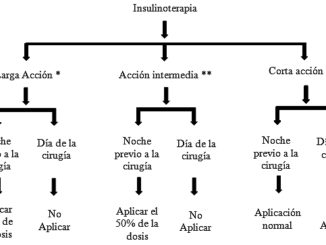
Administration of Anesthesia for removal of insulinoma is really challenging due to associated wide fluctuations in blood glucose levels perioperatively & during tumor handling. Any neurologic damage that has occurred as a result of previous hypoglycemic episodes or CIDP must be documented. Intravenous infusion of 5% Dextrose or 10% Dextrose should be started preoperatively to maintain blood glucose between 100-150 mg/dl. Diazoxide and somatostatin analogues are continued in the morning of surgery. Adequate NPO may not be achieved as patients may become symptomatic even after a few hours of fasting. Hence the risk of aspiration must be considered and full precautions should be taken[5 ].
Regarding Anesthetic agents for insulinoma enucleation, no specific recommendations are available. But since propofol has no effect on the release of insulin and glucose regulation, investigators advised combination of GA with propofol and epidural block. Enflurane and halothane inhibit pancreatic insulin release resulting in hyperglycemia[5 ].
Hypoglycemia may be masked under GA because signs of hypoglycemia can also occur due to hypovolemia, surgical stimulation, lighter surgical planes and pain. So, the main aim here is to prevent hypoglycemia until tumor resection and to control rebound hyperglycemia soon after resection. This is done by checking blood glucose before induction and every 15-30 minutes from then on to maintain plasma glucose in the desired range. It is imperative that glucose levels must be monitored in the recovery period also because risk of either: rebound hyperglycemia after resection (self-limiting persisting for few days) or hypoglycemia due to residual or missed adenomas that was not detected intraoperatively. Due to frequent blood sampling requirement, an arterial line is essential[5 ].
On the other hand, the choice of Anesthetic technique for patients with CIDP is complicated. We were unable to find clear recommendations on the Anesthetic management of these patients. If the patient has to be intubated, depolarising muscle relaxants must be avoided, however non-depolarising muscle relaxants can be used but monitoring of the relaxation is mandatory. Neuraxial techniques appear to be safe, bearing in mind the possibility of a larger block level than expected with subsequent impairment of respiratory function. With peripheral nerve block, the potential for direct nerve injury has to be considered. [6].
-
Conclusion
Though rare, when they do occur, these combined pathologies pose a great challenge to anesthesiologists. Vigilant monitoring of blood sugar intraoperatively is a must to counteract these wide swings and perioperative documentation of neurological data are very important hence providing a better patient outcome.
References
1. Jayasinghe KS, Nimalasuriya A, Dharmadasa K. A case of insulinoma with peripheral neuropathy. Postgrad Med J. 1983 Mar;59(689):189–90. https://doi.org/10.1136/pgmj.59.689.189 PMID:6302651
2. Ryan M, Ryan SJ. Chronic inflammatory demyelinating polyneuropathy: considerations for diagnosis, management, and population health. Am J Manag Care. 2018 Sep;24(17 Suppl):S371–9. PMID:30312032
3. Thomas J, Gupta S, Kilpadi K. Insulinoma-Anesthetic Implications with Review of Literature. J Anest & Intern Care Med. 2017;3(1):555605. https://doi.org/10.19080/JAICM.2017.03.555605.
4. Nockel P, Babic B, Millo C, Herscovitch P, Patel D, Nilubol N, et al. Localization of insulinoma using 68Ga-DOTATATE PET/CT scan. J Clin Endocrinol Metab. 2017 Jan;102(1):195–9. PMID:27805844
5. Goswami J, Somkuwar P, Naik Y. Insulinoma and anaesthetic implications. Indian J Anaesth. 2012 Mar;56(2):117–22. https://doi.org/10.4103/0019-5049.96301 PMID:22701200
6. Rivas BH, Romero RP, Sánchez JL. Anesthetic Options in Chronic Inflammatory Demyelinating Polyneuropathy. J Clin Case Rep. 2014;4(457):2.
7. Hsu YC, Zhan HL, Yang CP. Clinical and experimental evidence of hypoglycemic neuropathy. Diabetes Res Open Journal. 2015;1(5):131–5. https://doi.org/10.17140/DROJ-1-121.

 ORCID
ORCID