Edgardo Banille 1 ,*, Korbin Haycock 2 , Mariano Iriarte 1 , Alejandro Peirone 3 , Alejandro Contreras 3 , Florencia Muñoz 4 , Diego Rodríguez 5 , Verónica Selva 5 , Melanie Randall 2
Recibido: 12-11-2021
Aceptado: 10-12-2021
©2022 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 51 Núm. 2 pp. 221-224|https://doi.org/10.25237/revchilanestv5109021632
PDF|ePub|RIS
Utilidad de VExUS en paciente pediátrico portador de anomalía de Ebstein
Abstract
The venous excess ultrasound grading system (VExUS) is a relatively new application of point of care ultrasound. It has been successfully used to monitor for fluid overload in adult post-operative cardiac surgery patients. It has not been described in the management of congenital cardiac disease. We present a novel use of VExUS to diagnose decompensated Ebstein’s anomaly in a pediatric patient. A 13 year-old female with known stable Ebstein’s anomaly presented with new onset fluid overload and oliguria. Using abdominal venous Doppler ultrasound and VExUS, we were able to quickly differentiate the cause of the patient’s fluid overload as Ebstein’s anomaly instead of a primary renal etiology. This is the first reported use of VExUS to diagnose acute fluid overload in a pediatric patient with Ebstein’s anomaly. VExUS should be considered as a supplemental tool to diagnose fluid overload in other congenital cardiac diseases.
Resumen
El sistema de gradiente por ultrasonidos de exceso venoso (VExUS), es una aplicación relativamente nueva de los ultrasonidos en el punto de cuidado. Esto ha sido utilizado exitosamente para monitorizar la sobrecarga de fluidos en pacientes adultos en el período posoperatorio de cirugía cardíaca. No ha sido descripto en el manejo de las cardiopatías congénitas. Nosotros presentamos un novedoso uso de VExUS para diagnosticar una anomalía de Ebstein descompensada en un paciente pediátrico. Paciente femenina de 13 años de edad con una anomalía de Ebstein compensada en su evolución, se presenta con sobrecarga de fluidos y oliguria. Usando ultrasonidos Doppler de vasos abdominales (VExUS), fue posible diferenciar rápidamente la causa de la sobrecarga de fluidos en una anomalía de Ebstein que provoca insuficiencia renal. Este el primer caso reportado del uso del VExUS para el diagnóstico de sobrecarga de fluidos en pacientes pediátricos con anomalía de Ebstein. El score VExUS debería ser considerado como método complementario en el diagnóstico de la sobrecarga de fluidos en otras cardiopatías congénitas.
Ultrasound has been used and described increasingly to diagnose dynamic physiologic changes in patients in real time. Recently, the venous ultrasound excess grading system (VExUS) has been proposed and validated in an adult post cardiac surgery cohort[1]. Using hepatic, portal, and intra- renal venous Doppler tracings and assigning a score, venous congestion and fluid overload can be quickly diagnosed at the bedside.
Ebstein’s anomaly is a rare congenital malformation, comprising < 1% of all congenital heart disease[2]. The anomaly includes tricuspid valve malformation manifested as significant apical displacement of a dilated annulus and right ventricular dilation[2]-[4]. The most common features of worsening Eb- stein’s anomaly are arrhythmias, cyanosis, and right ventricular systolic deterioration. Traditionally, it is evaluated with standard echocardiography, chest radiograph, electrocardiogram, and cardiac magnetic resonance imaging[3].
A 13-year-old female presented to our outpatient pediatric cardiology clinic with two weeks of progressive lower extremity edema, dyspnea on exertion and oliguria. Her cardiac history consisted of complex left sided obstructive lesions including sub-aortic stenosis, aortic arch hypoplasia, aortic coarctation, left ventricular hypertrophy, and a restrictive intraventricular septal defect. She was also known to have Epstein’s anomaly which was clinically insignificant, having only mild tricuspid re- gurgitation. At two weeks of age, her aortic coarctation was corrected, and then at six months of age, she underwent angioplasty for re-coarctation. At one year of age, the patient had an aortic commissurotomy and wedge resection of the inferior intraventricular septum. She had annual echocardiography check-ups which showed stable mild tricuspid regurgitation.
At the time of presentation, the patient was afebrile, pale, and exhibited generalized edema including abdominal wall and upper and lower limbs. Her vital signs included a heart rate of 115 beats per minute, blood pressure of 115/65 millimeters of mercury, respiratory rate of 16 breaths per minute, and an oxy- gen saturation of 96%. She had a systolic 3/6 murmur, and her liver was palpated 2 centimeters (cm) below the costal margin. Laboratory testing showed a moderately elevated urine protein of 54 milligrams per deciliter (mg/dL) but a normal creatinine of 0.61 mg/dL and normal serum albumin of 3.73 grams/dL, making new onset nephrotic syndrome less likely. The fractional excretion of sodium was 0.26% pointing to a “prerenal” cause of oliguria. The B-type natriuretic peptide was significantly elevated at 7703 picograms per milliliter.
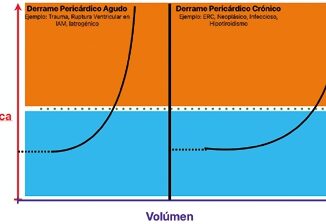
Echocardiography supplemented by hepatic and portal vein Doppler ultrasound ruled out intrinsic and extrinsic obstruction to the venous flow (pneumothorax, pericardial effusion, abdominal tumors, Budd-Chiari syndrome, and hepatic alterations). Color Doppler echocardiography indicated severe Eb- stein’s anomaly with significant dilatation of the right atrium (Figure 1). It showed a “Coanda effect” with systolic dysfunction of the right ventricle, estimated by the tricuspid annular plane systolic excursion of 15 cm, as well as tricuspid annular

Figure 1. Ebstein’s anomaly with significant dilatation of right atrium and right ventricle.
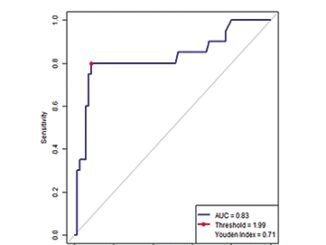
Using VExUS, the patient showed signs of severe venous congestion. First, the hepatic vein Doppler showed S wave reversal (Figure 2). While this finding will always be seen from the severe tricuspid regurgitation alone, her portal vein Doppler exhibited a pulsatility index of greater than 50% (Figure 3), and intra-renal venous Doppler showed a diastolic only interrupted flow pattern (Figure 4). All three of these Doppler findings together argued strongly for a severe venous congestive state. With this information, the patient was given hydrochlorothiazide 1 mg/kilogram/day and spironolactone 2 mg/kilogram/day. She initially had anuria but improved moderately. Cardiac catheterization and magnetic resonance imaging were performed, confirming severe tricuspid regurgitation and marked dysfunction of the left ventricle (ejection fraction: 25-30%), with likely grade two pulmonary hypertension. The left ventricular dyspeak systolic velocity of 8 cm per second. Diastolic dysfunction was also present. We identified new severe tricuspid regurgitation and extreme dilation of the inferior vena cava (2.9 cm), with nearly undetectable inspiratory collapse.

Figure 2. Hepatic vein Doppler with reversed systolic wave.
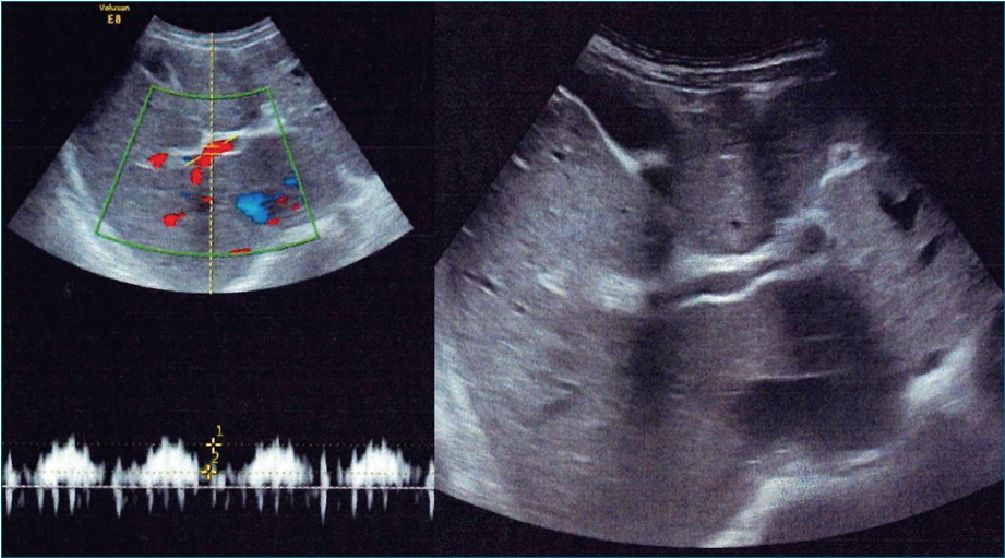
Figure 3. Portal vein Doppler showing with severe pulsatility

Figure 4. Intrarenal venous and arterial Doppler with interrupted diastolic venous flow and elevated renal resistive index of 0.8.
function and pulmonary hypertension likely contributed to the decompensation of her Ebstein’s anomaly. At the time of this writing, there are ongoing discussions of cardiac transplant for the patient.
Given the rarity of Ebstein’s anomaly, there are few studies of patients with acutely decompensated lesions. A longitudinal study following patients from fetal life to adulthood showed the presenting features to be cyanosis, heart failure, arrhythmia and abnormal fetal scan[5]. Acute kidney injury with generalized edema has not been previously described in this population.
The hepatic, portal, and intrarenal venous Doppler wave- forms, along with the intrarenal arterial Doppler waveforms give important immediate information as to the etiology of the renal dysfunction and edema. Perfusion of the organs depends not only on arterial pressure and flow, but also low venous
pressures. In contrast to the high elastance and resistive characteristics of systemic arterial vessels, the venous circulation is characterized by high capacitance, high compliance venules that can accommodate a large increase in blood volume. Venous flow patterns near to the right ventricle are characterized by waveforms determined by right atrial venous return dependent on right ventricular function and compliance as well as fluid volume status. Due to the normal compliant nature of the venous system, these pulsations are dampened in the veins dis- tant from the right ventricle and venous flow is more undulating and phasic in nature. Under situations of right ventricular failure, severe tricuspid regurgitation, or volume overload, the smaller veins become distended and non-compliant, causing them to transmit the pulsatile flow patterns seen in veins more proximal to the heart.
Conventional echocardiography complimented by the VExUS scoring system allowed our team to quickly diagnose de- compensated Ebstein’s and fluid overload. VExUS has been vali- dated in adult post cardiac surgical patients and has been used in a variety of both inpatient and outpatient settings, however we demonstrate its application in the novel case of congenital cardiac disease with acute kidney injury[6],[7].
Ethics approval: being a case report, this paper was exempt from our institutional review board.
Consent to participate: consent to publish all medical information was obtained in writing by the patient’s legal guardian.
Availability of data and materials: data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Competing interests: the authors declare that they have no competing interests
Funding: the authors declare that they have received no funding for this paper
1. Beaubien-Souligny W, Rola P, Haycock K, Bouchard J, Lamarche Y, Spiegel R, et al. Quantifying systemic congestion with Point-Of-Care ultrasound: development of the venous excess ultrasound grading system. Ultrasound J. 2020 Apr;12(1):16. https://doi.org/10.1186/s13089-020-00163-w PMID:32270297
2. Attenhofer Jost CH, Connolly HM, Dearani JA, Edwards WD, Danielson GK. Ebstein’s anomaly. Circulation. 2007 Jan 16;115(2):277-85. . 106.619338. https://doi.org/10.1161/CIRCULATIONAHA.106.619338.
3. Holst KA, Connolly HM, Dearani JA. Ebstein’s Anomaly. Methodist DeBakey Cardiovasc J. 2019 Apr-Jun;15(2):138–44. https://doi.org/10.14797/mdcj-15-2-138 PMID:31384377
4. Qureshi MY, O’Leary PW, Connolly HM. Cardiac imaging in Ebstein anomaly. Trends Cardiovasc Med. 2018 Aug;28(6):403–9. https://doi.org/10.1016/j.tcm.2018.01.002 PMID:29409687
5. Celermajer DS, Bull C, Till JA, Cullen S, Vassillikos VP, Sullivan ID, et al. Ebstein’s anomaly: presentation and outcome from fetus to adult. J Am Coll Cardiol. 1994 Jan;23(1):170–6. https://doi.org/10.1016/0735-1097(94)90516-9 PMID:8277076
6. Beaubien-Souligny W, Bouchard J, Desjardins G, Lamarche Y, Liszkowski M, Robillard P, et al. Extracardiac Signs of Fluid Overload in the Critically Ill Cardiac Patient: A Focused Evaluation Using Bedside Ultrasound. Can J Cardiol. 2017 Jan;33(1):88–100. https://doi.org/10.1016/j.cjca.2016.08.012 PMID:27887762
7. Mahmud S, Koratala A. Assessment of venous congestion by Doppler ultrasound: a valuable bedside diagnostic tool for the new-age nephrologist. CEN Case Rep. 2020 Jul;•••: https://doi.org/10.1007/s13730-020-00514-5 PMID:32734585

 ORCID
ORCID