Mariana R. Rojas4, Lucile Gignon M.D., M.Sc.3,4, Fernando Díaz1,*, Andrei Florea M. Bmed Sci2, Patricio A. Leyton M.D., M.Sc. Medical Education3,4, Juan Abarca Z. M.D.3,4, Javiera Vargas Z. M.D., Mg.3,5
Recibido: 23-10-2021
Aceptado: 11-03-2022
©2022 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 51 Núm. 4 pp. 395-399|https://doi.org/10.25237/revchilanestv5111051114
PDF|ePub|RIS
Extubación precoz en pacientes con neumonía por COVID-19 y cambios en el perfil temporal de LDH
Abstract
Since the beginning of the 2019 global pandemic of Coronavirus Disease, using invasive mechanical ventilation as support therapy has been a critical treatment of acute respiratory failure. In the context of a collapsed health system, having an early extubation predictor becomes a useful way of supporting clinical management, by enabling to anticipate the availability of mechanical ventilators. Hence, we assessed the relationship between the progression of lactate dehydrogenase and early extubation in patients with COVID-19. A retrospective study. A single private hospital in Chile. Adults aged 18 or older diagnosed with COVID-19 pneumonia and requiring mechanical ventilation, having been admitted to an ICU during the study period. None. Fifty two individuals, 73% males, were included with a median age of 47.1 years old and a median body mass index of 29. Individuáis extubated within the first 5 days of mechanical ventilation, early extubation group, amounted to 34.6%. The average decrease in serum lactate dehydrogenase levels was 27.5 UI/L per day (p < 0.01) in the early extubation group compared to 14.7 UI/L per day (p < 0.01) in the late extubation group (individuals extubated after day 5). During the first 48 hours, the average daily decrease was 56.7 UI/L in the early extubation group compared to 13.2 UI/L per day in late extubation group (p < 0.01). Serum lactate dehydrogenase daily level decrease during the first days of mechanical ventilation is associated with earlier patient extubation.
Resumen
Desde inicios de la pandemia de 2019 de enfermedad por Coronavirus, la terapia de soporte con ventilación mecánica invasiva ha sido fundamental en el tratamiento de la falla respiratoria aguda. En contexto de un sistema de salud saturado, es útil contar con un predictor de extubación precoz para apoyar el manejo clínico, al anticipar disponibilidad de ventiladores mecánicos. Por lo tanto, evaluamos la relación entre progresión de lactato deshidrogenasa y extubación precoz en paciente cursando con COVID-19. Estudio retrospectivo. Centro único, hospital privado en Chile. Adultos mayores o igual a 18 años, con diagnóstico de Neumonía por COVID-19 y requerimientos de ventilación mecánica, ingresado a UCI durante el período estudiado. No. Fueron incluidos cincuentas y dos individuos, 73% de sexo masculino, con una mediana de 47,1 años de edad e índice de masa corporal de 29. El grupo de extubación precoz, individuos extubados dentro de los 5 primeros días de ventilación mecánica, correspondió al 34,6%. El descenso promedio de lactato deshidrogenasa en el grupo de extubación precoz fue de 27,5 UI/L diario (p < 0,01), comparado con 14,7 UI/L diario en el grupo de extubación tardía (individuos extubados posterior al día 5 – p < 0,01). En las primeras 48 horas el descenso promedio en el grupo de extubación precoz fue 56,7 UI/L diario, comparado con 13,2 UI/L diario en el grupo de extubación tardía (p < 0,01). El descenso diario del nivel sérico de lactato deshidrogenasa en los primeros días de ventilación mecánica se asocia con una extubación precoz.
-
Introduction
The Coronavirus-19 (COVID-19) pandemic has had a huge impact on health worldwide. Although most infected people develop a mild disease, approximately 5% of individuals may present with acute respiratory distress syndrome (ARDS) and multiple organ failure, requiring mechanical ventilation (MV) and management in an intensive care unit (ICU)[1]. Ventilatory support is key for management but is associated with complications. MV-associated lung injury and MVassociated pneumonia are more likely to occur with each day after in- tubation[2]. Therefore, patient prompt extubation is imperative for providing tremendously needed mechanical ventilators. To this end, it is useful to have a biomarker that serves as guideline and support for decision making.
Several biomarkers have been studied looking to help clinicians to make better decisions based on mortality and severity grading quantitative predictors[3],[4]. Lactate dehydrogenase (LDH) is an intracellular enzyme involved in anaerobic glycolysis and widely found in almost all living tissues. LDH levels aug- ment in several conditions such as tissue injuries, inflammation, and hemolysis[5]. COVID-19 related increase in LDH levels are associated with higher rates of complications and mortality[3]. LDH has not yet been studied as a biomarker to predict early extubation, nevertheless, nor has been examined whether is as- sociated with reductions in MV-related comorbidities[2].
In this study, we assessed the progress of LDH levels during mechanical ventilation and how it relates to early extubation in COVID19 acute respiratory failure patients.
-
Materials and Methods
This retrospective study included a cohort of patients diag- nosed with COVID-19 pneumonia requiring MV. It was con- ducted at Clínica Alemana de Santiago in converted ICUs man- aged by anesthesiologists, during the second COVID-19 wave in Chile (March to July 2021). The protocol of the study was approved by the ethic committee of Clínica Alemana de Santiago, with the exception of the informed consent due to the exceptional pandemic situation [Approval N° 2020-35].
Patients included in this study were 18 years old or older with a COVID-19 acute respiratory failure requiring MV support. Exclusion criteria were presence of pulmonary embolism (PE) (diagnosed by imaging methods), active cancer, death within 5 days of MV, and clinical evidence of myocarditis or rhabdomyolysis. We searched for the ability of LDH levels to predict early extubation. Patients extubated within the first 5 days of tracheal intubation were classified as early extubation group, while patients extubated from day 6 and after were classified as late extubation group. Data was adjusted by the following factors: patients’ baseline characteristics (age, body mass index [BMI], SOFA score), noninvasive ventilation (NIV) support before intubation, daily doses of methylprednisolone, volume of com- promised lung on a Computed Tomography (CT) scan (less or more than 30%), aspartate aminotransferase (AST), total bilirubin at the start of MV, and daily serum LDH measured for the first 7 days.
The analysis of continuous variables between groups was made with MannWhitney’s or Student’s T tests, depending on their distribution. We compared categorical variables by means of the ChiSquare or Fisher’s exact tests, as appropriate. We built a logistic model to analyze the association between early extubation and factors. Mixed models were used for the analysis of LDH levels, using the day of measurement as the time variable. We also used mixed models for covariance analysis to estimate early extubation; LDH level was the response variable, time the continuous variable, and early extubation the differentiating factor (considering p < 0.05 as significant).
-
Results
Of the 60 COVID-19 patients requiring MV admitted into the converted ICU’s, 8 were excluded according to the defined criteria (6 PE cases and 2 deceased). The median age of the 52 patients enrolled was 47.1 years (SD ±12.5), and a mean BMI of 29 (26.5-32.4). Males amounted to 73% of the patients. Involvement over 30% of the lung in pulmonary CT scans were present in 58% of the patients. NIV support before intubating was established in 92% of the patients. The preintubation PaO2/FiO2 ratio was 206 (172-257). Methylprednisolone pulses were administered to 86% of the patients. Table 1 describe the characteristic of both groups.
The percentage of early extubated patients was 34.6%, with a significant relationship to age both in the univariate and multivariate analysis models. Early extubation did not significantly relate to NIV support before intubation, use of corticoids, CT lung involvement, PaO2/FiO2 ratio, or SOFA and Apache scores. The late extubation group did show more ICU hospitalization days than early extubation group with a statistically difference. Reintubation cases, tracheostomy and infection cases did not show difference.
Table 1. Describe the characteristic of both groups
| Early extubated | Late extubated | OR [IC 95%] | P Value | |
| Age (years) | 41.4 (SD ± 11.6) | 50.2 (SD ±11.9) | 0.95 [0.88-0.99] | < 0.01 |
| BMI (Kg/Mt2) | 29.3 (SD ± 4.2) | 30.9 (SD ±5.3) | 0.3 | |
| Male | 61 % | 79% | 0.15 | |
| NIV support pre-intubation | 94% | 91% | 0.59 [0.03-10.14] | 0.67 |
| SOFA score | 3(2-3) | 3(2-5) | 0.08 | |
| APACHE score | 4(2-7) | 5(3-8) | 0.27 | |
| Compromise > 30% of lung tissue | 75% | 64% | 1.66 [0.42-6.56] | 0.46 |
| Pre intubation PaO2/FiO2 ratio | 261 (SD ± 62) | 247 (SD ± 83) | 1.00 [0.99-1.01] | 0.58 |
| Methylprednisolone pulse | 78% | 91% | 0.33 [0.06-1.71] | 0.17 |
| Days between hospitalizaron and intubation | 1 (0-1) | 1 (0-2) | 0.46 | |
| Days between start of symptoms and intubation | 8 (7-11) | 9 (8-11) | 0.67 | |
| ICU hospitalizaron days | 5(4-5) | 9 (7-11) | < 0.01 | |
| Reintubation cases | 0 | 4 | 0.12 | |
| Tracheotomy cases | 0 | 2 | 0.29 | |
| Infection cases | 2 | 10 | 0.13 |
Temporal changes in LDH levels were not associated to liver enzyme or total bilirubin levels – dichotomized to twice the top normal value in the univariate model – when measured at the beginning of MV or at 72 hours after intubation.
The preintubation level of LDH showed a significant relationship with the CT lung involvement. Levels of LDH were 112.4 UI/L higher in the group of patients with lung involve- ment > 30% (p = 0.01), with a significant decrease 24 hours postintubation (p < 0.03).
LDL levels were not different at baseline between early and late extubation groups (p = 0.19) (Figure 1A). LDL levels de- creased over time significantly in both early and late extubation groups. The average LDH level decrease in the early extubation group was 27.5 UI/L per day (p < 0.01) while 14.7 UI/L per day in the late extubation group (p < 0.01) (Figure 1A). The assessment of the LDH drop gradient during the first 48 hours showed an average drop of de 56.7 UI/L (p < 0.01) in the case of the early extubated group, versus 13.2 UI/L per day for the late extubated one (Figure 1B).
-
Discussion
Previous studies have established that high initial levels of LDH are a biomarker of worse prognosis in COVID-19 infection[7]. We show that time-course levels of LDH during first days after intubation are useful to predict early extubation. Mechanically ventilated patients exhibiting a more pronounced decrease in LDH levels during the first 5 days of MV, have an association with earlier extubation compared to those patients with a less pronounced reduction. This suggests that the serial control of this biomarker may be considered in the clinical decision-making process of these patients. Considering this center’s patient management, the LDH trend can support decisions on dose adjustments of sedation and neuromuscular blocking drugs.
Baseline LDH levels were higher in patients with a greater than 30% lung involvement measured by CT scans. This finding is likely in response to the degree of cell damage, as is also the case in lung fibrosis[8]. Decrease in LDH levels after 24 hours of MV may reflect the lung protector effect of MV. However, we know that patients benefit from other intervention as well. We have observed that early NIV support as a bridge to MV or no delay in intubation when necessary, improves outcomes. Patients also benefit from well systematized management pro- tocol including early initiation of methylprednisolone pulses. ClimenteMartini et al.[9], demonstrated the beneficial effect of methylprednisolone with less mortality in severe cases (HR of 0.11).
As expected, the late extubation group had significantly more ICU hospitalization days than early extubation group. They had also more reintubation, tracheostomy, and infection cases, but without statistically significance.
LDH levels did not show a relation to liver tests and hence were not considered in the multivariate analysis. Notably, liv- er function tests are not associated with death or MV dura- tion[10]. We considered other laboratory tests and vital signs concentrated in severity scores as APACHE and SOFA, both without statistical differences between groups.
There was no accountable death within 30 days in the sample, excepting the two patients excluded for early death. We don’t have an explanation for this low mortality, probably because a small sample size. Another explanation could be the way we have been working in this ICU with well systematized management protocol that includes a NIV support, early intubation and prono ventilation, high corticoids doses, active searching and treatment of infection, appropriate nutrition and boost the intestinal transit.
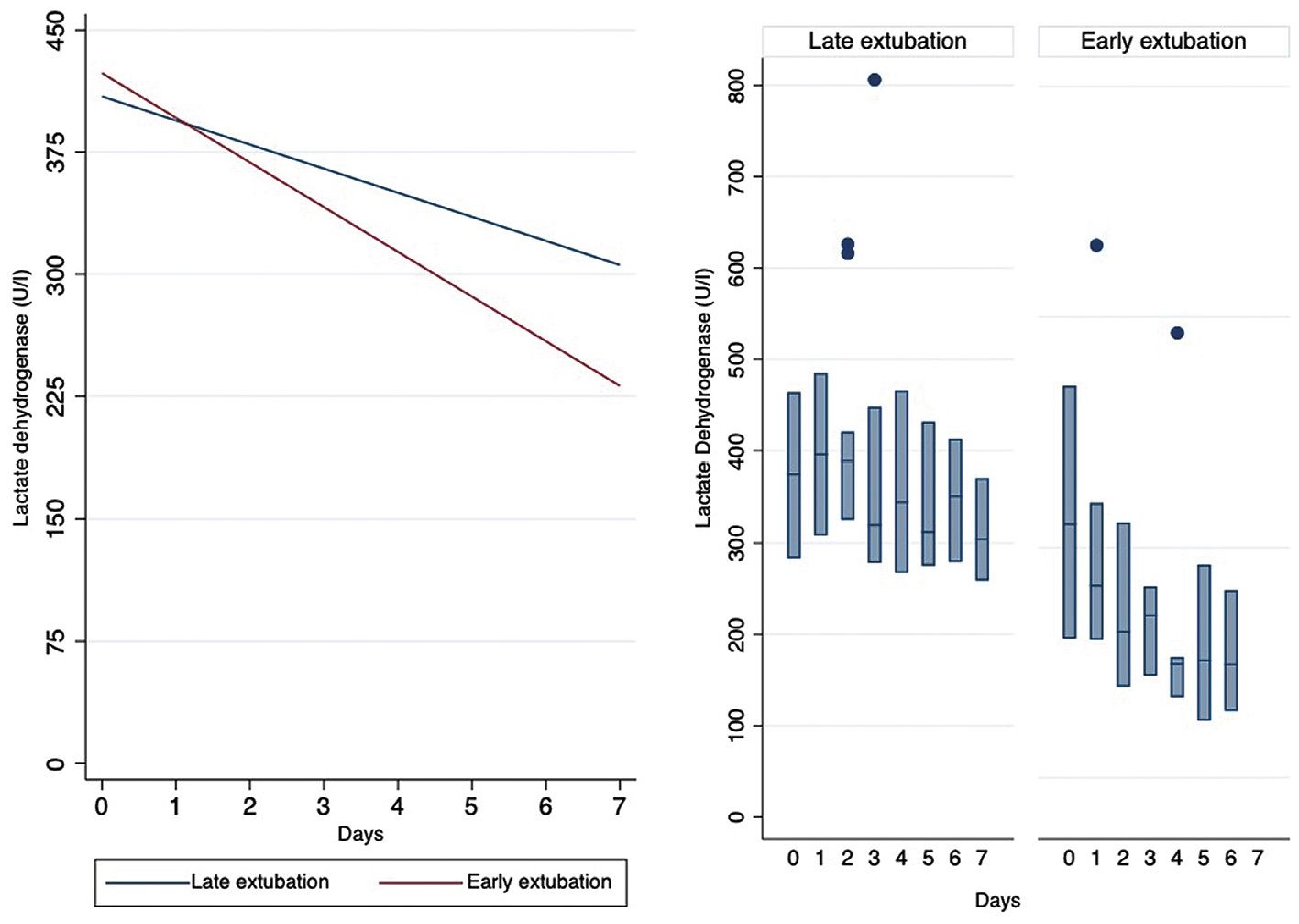
Figure 1. Predicted and Observed Lactate Levels of Dehydrogenase. 1A: Curves of Predicted LDH Levels in the Late and Early Extubated Groups. 1B: Box Diagram of Observed LDH Levels in the Late and Early Extubated Groups, Showing the 25th to 75th Percentiles and Outliers.
Limitations in our study were a small sample size of patients from a single unit of our center. Another limitation relates to LDH broad tissue distribution making questionable the origin of the elevation of LDH levels. Should we find a lungspecific biomarker that better distinguishes the trends of patient evolution, thus eliminating confusing factors that can raise LDH levels, is still and ideal open demand. Nonetheless, the main advantage of well-known LDH tests is its worldwide, fast and low cost availability. Currently health systems need simple and afford- able solutions to help clinicians take better care of COVID-19 patients.
-
Conclusion
Patients showing a pronounced daily reduction in LDH levels during the first days of MV are more likely to be extubated earlier than patients with smaller reductions. LDH serial quanti- fications may more completely enlighten clinicians’ extubation decision making process.
Acknowledgments: We thank the respiratory therapists and critical care nurses of the Medical ICU at Clínica Alemana de Santiago.
Contribution of the authors: Vargas J. conceived the study design and performed the statistical analysis. All authors participated on the acquisition of data, argumentation and writing of the manuscript. Rojas M. edited the manuscript with input from all authors. Gignon L., Leyton P. and Rojas M. performed a critical review of the intellectual content, supervised by senior anesthetist Abarca J. Final manuscript was read and approved by all authors.
Institution: Clínica Alemana de Santiago.
Conflicts of Interest: All the authors have disclosed that they do not have any conflicts of interest.
Financial Support: The Clinical Trial and Research Unit of the Department of Academic Development and Research of Clínica Alemana de Santiago financed both the field researchers contributions and consulting for translation into English.
References
1. Tan E, Song J, Deane AM, Plummer MP. Global Impact of COVID-19 Infection Requiring Admission to the Intensive Care Unit: A Systematic Review and Meta-Analysis. Chest. 2020;159(2):524536. PMID:33069725
2. Blot S, Koulenti D, Dimopoulos G, Martin C, Komnos A, Krueger WA, et al.; EU-VAP Study Investigators. Prevalence, risk factors, and mortality for ventilator-associated pneumonia in middle-aged, old, and very old critically ill patients. Crit Care Med. 2014 Mar;42(3):601–9. https://doi.org/10.1097/01.ccm.0000435665.07446.50 PMID:24158167
3. Martha JW, Wibowo A, Pranata R. Prognostic Value of Elevated Lactate Dehydrogenase in Patients with COVID19: A Systematic Review and MetaAnalysis. Postgrad Med J. 2021;0:16. PMID:33452143
4. Kermali M, Khalsa RK, Pillai K, Ismail Z, Harky A. The role of biomarkers in diagnosis of COVID-19 – A systematic review. Life Sci. 2020 Aug;254:117788. https://doi.org/10.1016/j.lfs.2020.117788 PMID:32475810
5. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 Mar;395(10229):1054–62. https://doi.org/10.1016/S0140-6736(20)30566-3 PMID:32171076
6. Lu J, Wei Z, Jiang H, Cheng L, Chen Q, Chen M, et al. Lactate dehydrogenase is associated with 28-day mortality in patients with sepsis: a retrospective observational study. J Surg Res. 2018 Aug;228:314–21. https://doi.org/10.1016/j.jss.2018.03.035 PMID:29907227
7. Chen XY, Huang MY, Xiao ZW, Yang S, Chen XQ. Lactate dehydrogenase elevations is associated with severity of COVID-19: a meta-analysis. Crit Care. 2020 Jul;24(1):459. https://doi.org/10.1186/s13054-020-03161-5 PMID:32709251
8. Åttingsberg E, Hoyer N, Wilcke T, Skovhus T, Bendstrup E, Shaker S. Lactate Dehydrogenase as a Biomarker of Advanced Disease in Idiopathic Pulmonary Fibrosis. Eur Clin Respir J. 2019;54:PA4701.
9. Climente-Martí, M, Ruiz-Millo, O, López-Cruz, I, et al. Impact of intermediate to high doses of methylprednisolone on mortality rate in patients with COVID-19 pneumonia-induced severe systemic inflammation. Int J Clin Pract. 2021; 75:e14479. https://doi.org/10.1111/ijcp.14479
10. Elmunzer BJ, Spitzer RL, Foster LD, Merchant AA, Howard EF, Patel VA, et al.; North American Alliance for the Study of Digestive Manifestations of COVID-19. Digestive Manifestations in Patients Hospitalized With Coronavirus Disease 2019. Clin Gastroenterol Hepatol. 2021 Jul;19(7):1355–1365.e4. https://doi.org/10.1016/j.cgh.2020.09.041 PMID:33010411

 ORCID
ORCID