Matías Ramos M.D.1,*
Recibido: 11-01-2022
Aceptado: 22-04-2022
©2023 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 52 Núm. 1 pp. 9-10|https://doi.org/10.25237/revchilanestv5208111559
PDF|ePub|RIS
¿Intubación esofágica? ¡Mire sus monitores!»
-
To the editor,
Intelligent design is a form of creationism that argues for an intelligent cause behind the complexity of human beings and against natural selection as an evolutionary force. If so, what kind of intelligent designer could be behind the fact that in our anatomy the airway and the digestive tract share structures? With this “design”, the supposed “engineer” exposes us to obstructions and suffocation because, in a small space, the ventilatory flow and the food bolus must be directed by parallel paths arranged side by side but totally different.
In the field of airway management, this anatomical arrangement is the source of a serious complication: undetected esophageal malposition of an endotracheal tube can be devastating[1].
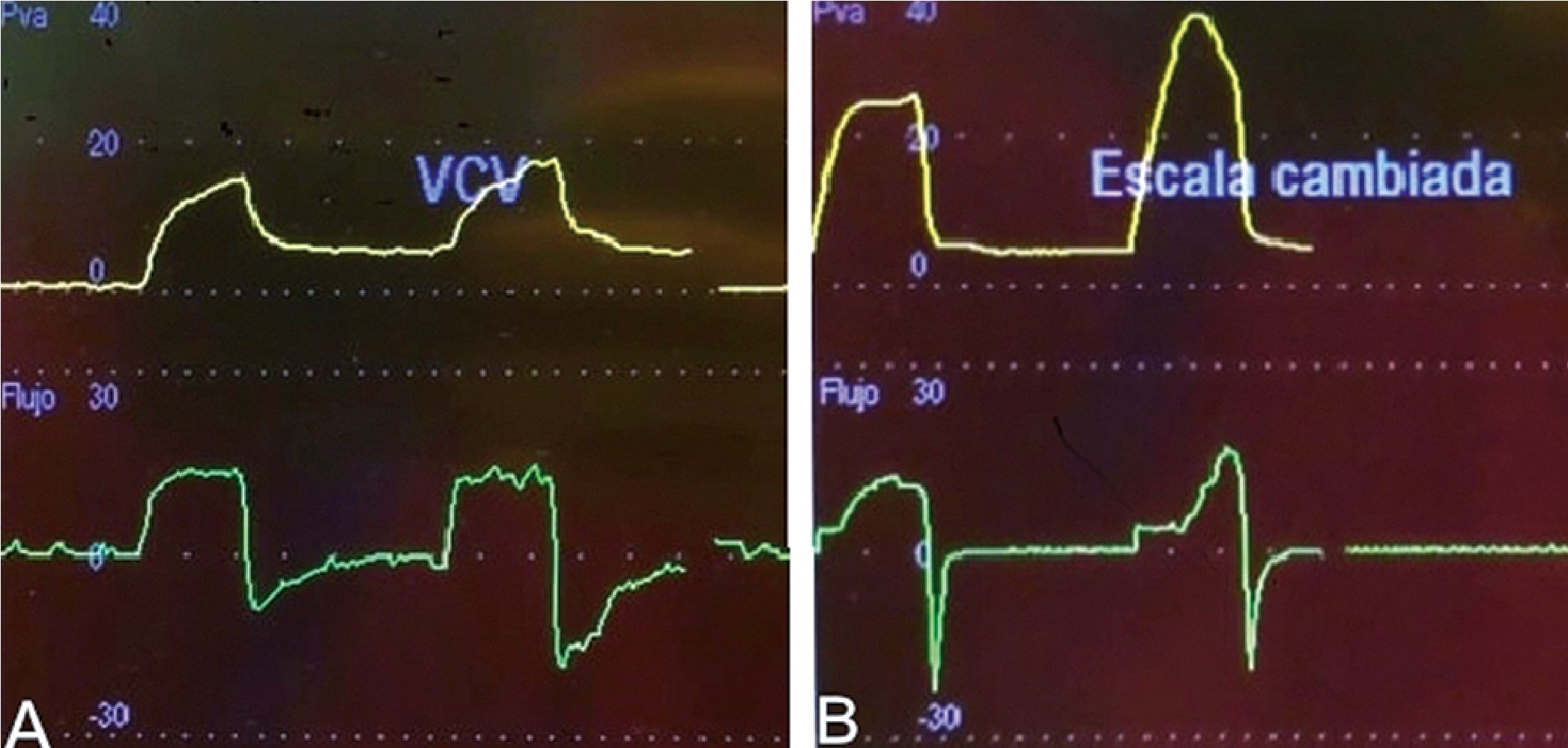
Figure 1. First and second ventilatory curves of a tracheal (A) and esophageal (B) intubation. Upper half: pressure-time curves. Lower half: flow-time curves. Ventilatory settings: tidal volume 400 ml, I:E 1:2, PEEP 5 cmH2O.
The confirmation of tracheal intubation is a dual process since it is not only necessary that the tube is in the airway, but that it is in the correct position within it[2]. It is also a dynamic process, especially in the operating room, where the patient is exposed to positional changes, tractions and procedures in the oral cavity that can misposition or even remove a correctly placed and positioned endotracheal tube.
No method of confirming intubation is perfectly sensitive and specific in all age ranges and circumstances, thus the combination of various methods and clues are used to determine with an acceptable range of confidence that the tube is in the correct place. These methods, with different predictive values, can be classified in different ways: they can be objective or subjective, require the start of ventilation, depend on pulmonary blood flow, etc.
During positive pressure ventilation, exhalation is a passive phenomenon that depends on the mechanical properties of the structure that returns the insufflated volume, specifically its elasticity and resistance[3]. The mechanical properties of the lungs and trachea are markedly different from those of the stomach and esophagus. In this way, the rapid feedback that we obtain from the pressure and flow monitors after the first and even second insufflation of the ventilator could guide us on the position of the endotracheal tube. By analyzing the morphology of the expiratory flow, one can infer the elastic and resistive properties of the exhaling structure[4]. Figures 1-A and 1-B show the pressure-time and flow-time curves in volume control ventilation corresponding to tracheal and esophageal intubation, respectively.
It can be noted that pulmonary exhalation is a process with a slower and more arranged exponential decay than gastric “exhalation”, which is more abrupt and truncated (possibly due to esophageal collapse).
After intubating and connecting the patient to the ventilator, one could observe the movement of the chest and the condensation of the tube. Then quickly interpret the first expiratory curve during the seconds it takes for the first capnographic trace to appear (or not). Like good pilots, we must learn to trust our instruments as much as our eyes[5].
Although the delay of sidestream capnography is in the order of seconds, in situations where this technology is not available or the pulmonary flow is inadequate (intubation during cardiac arrest), the visualization of the expiratory curves could provide fast, objective and complementary information to other intubation confirmation methods.
References
1. Hagberg C, Georgi R, Krier C. Complications of managing the airway. Baillieres Best Pract Res Clin Anaesthesiol. 2005 Dec;19(4):641–59. https://doi.org/10.1016/j.bpa.2005.08.002 PMID:16408539
2. Straker T, Urdaneta F. Confirmation of Tracheal Intubation. In: Hagberg CA, editor. Benumof’s and Hagberg’s Airway Management. 4th ed. Philadelphia (PA): Elsevier Saunders; 2018.
3. Goebel U, Haberstroh J, Foerster K, Dassow C, Priebe HJ, Guttmann J, et al. Flow-controlled expiration: a novel ventilation mode to attenuate experimental porcine lung injury. Br J Anaesth. 2014 Sep;113(3):474–83. https://doi.org/10.1093/bja/aeu058 PMID:24694683
4. Guttmann J, Eberhard L, Fabry B, Bertschmann W, Zeravik J, Adolph M, et al. Time constant/volume relationship of passive expiration in mechanically ventilated ARDS patients. Eur Respir J. 1995 Jan;8(1):114–20. https://doi.org/10.1183/09031936.95.08010114 PMID:7744177
5. Perrone JA. Visual slant misperception and the ‘black-hole’ landing situation. Aviat Space Environ Med. 1984 Nov;55(11):1020–5. PMID:6508682

 ORCID
ORCID
 Creative Commons Attribution
Creative Commons Attribution