Diana Sarmiento MD.1, María José Andrade López MD.2,*, Andrea Casanova3, Isabella Garavis2, Lizeth Castro MD.3
Recibido: 26-04-2023
Aceptado: 30-06-2023
©2023 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 52 Núm. 6 pp. 626-628|https://doi.org/10.25237/revchilanestv52n6-12
PDF|ePub|RIS
Manejo perioperatorio de ganglioneuroblastoma torácico
Abstract
We present the case of a 20-month-old patient with a ganglioneuroblastoma, who had received two cycles of chemotherapy, and in whom it was decided to resect the tumor via thoracotomy. It was found that the tumor was firmly adhered to the aortic arch, left carotid artery and roots of thoracic nerves, however a 99% tumor resection was achieved. We want to highlight the importance of this anesthetic challenge that this case represented in the perioperative period due to the delicate state of the patient as well as the abundant use of hemodynamic monitoring technology throughout the procedure.
Resumen
Presentamos el caso de un paciente de 20 meses con un ganglioneuroblastoma, que había recibido dos ciclos de quimioterapia, en el que se decidió extirpar el tumor mediante toracotomía. Se encontró que el tumor estaba firmemente adherido al arco aórtico, arteria carótida izquierda y raíces de los nervios torácicos, sin embargo, se logró una resección del 99% del tumor. Queremos resaltar la importancia de este desafío anestésico que representó este caso en el perioperatorio debido al delicado estado del paciente, así como al abundante uso de tecnología de monitoreo hemodinámico durante todo el procedimiento.
-
Introduction
Ganglioneuroblastoma is an uncommon malignant tumor of the sympathetic nervous system that arises from the primitive sympathogonia[1]. The tumor is composed of mature gangliocytes and immature neuroblasts and has an intermediate malignant potential[1]. They can grow in places such as the adrenal medulla, extra-adrenal retroperitoneum, posterior mediastinum, and the neck[1]. This tumor is common in children between the age of 1-2 years old, and the usual median age is 22 months[2]. The clinical presentation of this type of tumors can include pain because of the local effects of the primary tumor, abdominal distention, irritability, weight loss, shortness of breath in the case of a large tumor[1].
We present the case of a 22-months-old patient diagnosed with ganglioneuroblastoma who received two cycles of chemotherapy in whom resection of the tumor was made. The localization of the tumor was in the posterior mediastinum, and was firmly attached to the aortic arch, left carotid and thoracic nerve roots. In the following article we want to highlight the anesthetic challenge that this case represents in the perioperative period due to the characteristics of the tumor, and the demographic characteristics of the patient.
-
Case
A 22-month-old patient who came to a tertiary care hospital with her father with a posterior mediastinal tumor biopsy, which was identified as a ganglioneuroblastoma. At the moment the patient was asymptomatic, and on physical examination she was in adequate general conditions. Images are reviewed in which the tumor of 7 cm x 4 cm is found in the posterior mediastinum (Figure 1). At this time, the patient had already received two cycles of chemotherapy for cytoreduction, and the third cycle was suspended due to non-response to treatment, for which she was scheduled for tumor resection.
The pre-anesthetic assessment showed a Mallampati of I, ASA status of III, with low cardiovascular risk, low possible requirement of blood products and with medium surgical risk.
Initially, posterior mediastinal tumor resection by thoracoscopic was undergone to evaluate characteristics and possible adhesions, with subsequent decision to convert to open surgery via thoracotomy, due to firm adhesions to the aortic arch, left carotid artery and thoracic nerve roots and additional closed thoracostomy for drainage. Upon admission to the operating room, remifentanil 0.2 mcg/kg/min and hydromorphone hydrochloride 0.05 mg IV were administered. Surgery was performed without complications, with findings of posterior mediastinum tumor firmly adhered to vital structures described. It was decided to monitor the patient in the pediatric intensive care Unit, maintaining sedoanalgesia with fentanyl infusion, invasive mechanical ventilatory support, and antibiotic prophylaxis; and eventual subsequent extubation was performed. Three days after the surgical procedure the patient was discharged from the PICU and transferred to the pediatric wing, with later removal of the chest tube without complications.
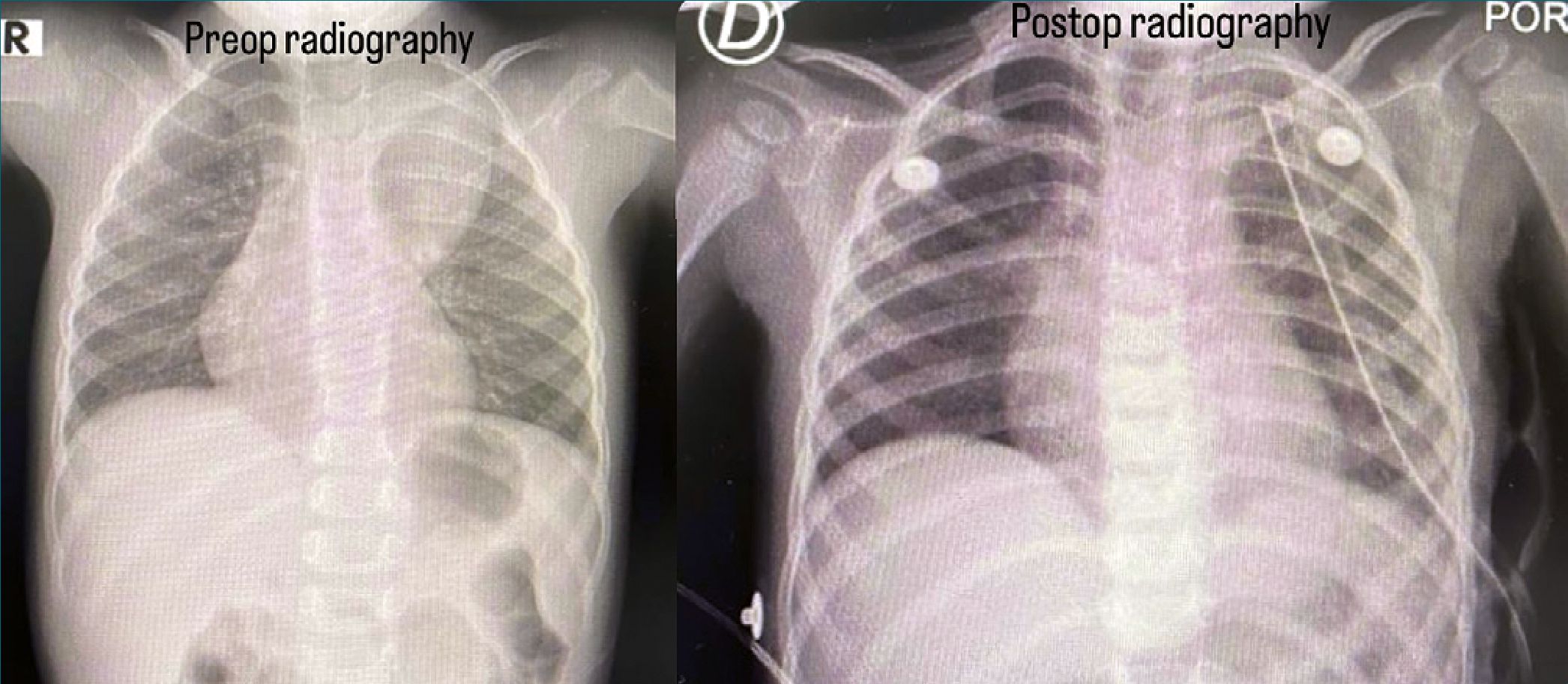
Figure 1. Preoperative and postoperative chest x-ray.
-
Discussion
The ganglioneuroblastoma (GNB) is a rare malignant tumor of the sympathetic nervous system, and is considered a disease of the child population, with most cases in patients under four years of age, especially in ages 1 to 2 years, with a median of age at diagnosis of 22 months[2],[3]. Additionally, the most common sites of origin are the adrenal medulla (about 35%), the extra-adrenal retroperitoneum (30%-35%), and the posterior mediastinum (20%)[1],[3]. Our case shared many similarities with what is currently established in the literature, such as the time of presentation and the tumor was found in the posterior mediastinum which is a relatively common site.
Tomography (CT) and magnetic resonance imaging are the most widely used imaging methods for the evaluation of GNB[1], however our diagnosis was through clinical suspicion and subsequent imaging confirmation by chest X-ray, and histopathological study after surgical resection[4]. The characteristics of GNB are variable on contrast-enhanced CT, from oblong and well-defined paravertebral masses with homogeneous enhancement to irregular, cystic, hemorrhagic, or locally invasive[5]. In the case of our patient, she presented firm adhesions to the aortic arch, left carotid artery and thoracic nerve roots. Approximately 50% of thoracic GNB/neuroblastomas have thick, finely dotted, or curvilinear calcifications[1], which was not evidenced in our patient.
Early and radical surgery is the best treatment available for mediastinal NGB. The prognosis is generally favorable with two- year and five-year survival rates of 92% and 88%, respectively[6]. Adam and Hochholzer[6] demonstrated that recurrence in GNB of the posterior mediastinum after surgery occurred only in adult/adolescent patients, which is favorable for the prognosis of the case presented. In general, older children with neuroblastoma/GNB had worse outcomes compared to younger children[7],[8].
Mediastinal GNBs are better in terms of prognosis than those of the abdomen, since patients with the former tend to be diagnosed earlier, when the size is still small and, therefore, complete resection of the tumor is possible[9]. Complete resection remains the mainstay of treatment for localized mediastinal neuroblastomas[9]. There are no reports of the recommended duration of follow-up; however, follow-up with a chest X-ray is required, taking the immediate postoperative X-ray as a reference, as was done in the case described. Two-year event-free survival rates are 85% to 100%; relapses can be managed with surgery of the new lesion or chemotherapy[10].
Regarding anesthetic considerations, many important physiological alterations can be related to the position of the patient and the insufflation of air or CO2 in the body cavities during thoracoscopy[11], which was initially performed by the surgical team in our case. Although extremely rare, air embolism can occur during such procedures and also must be taken into account[11]. The understanding of the anticipated procedure combined with the knowledge of its effects on cardiorespiratory function must be carried out in order to have adequate anesthetic planning[11],[12]. Depending on the location and extension of the mass at the level of the mediastinum, ventilation techniques with single lumen tubes or single lung ventilation may be chosen in adolescents, since this group tends to tolerate the complete collapse of one lung and is particularly optimal for procedures that require exposure of the mediastinum and for pleurodesis[13]. General anesthesia with two-lung ventilation can be used in any age group, but is usually necessary for infants and young children, as they often will not tolerate collapse of one lung, and in older children or adolescents with severe lung compromise[13]; therefore, it was the decision made by the anesthesia team in our case.
In summary, we describe this particular case of a GNB of the posterior mediastinum, which is normally common within this group of pathologies, but with certain anatomical challenges such as firm adherence to the aortic arch, left carotid artery and thoracic nerve roots. which made the hemodynamic management more delicate.
-
Conclusions
– GNB is a rare tumor, however, it occurs in the pediatric population with most cases in patients under 4 years of age, like our case in which our patient was 22-months old.
– This case was considered a challenge due to the location of the tumor, since it was firmly adhered to the aortic arch, left carotid artery and the roots of the thoracic nerves, being important structures and delicate to handle.
– Management was considered satisfactory in terms of anesthetic procedure, extubation and successful pain management. Additionally, there were no complications or physiological alterations related to the thoracoscopy, with an adequate evolution of the patient.
References
1. Lonergan GJ, Schwab CM, Suarez ES, Carlson CL. Neuroblastoma, ganglioneuroblastoma, and ganglioneuroma: radiologic-pathologic correlation. Radiographics. 2002;22(4):911–34. https://doi.org/10.1148/radiographics.22.4.g02jl15911 PMID:12110723
2. Sekiguchi N, Noguchi T, Fukushima T, Kobayashi T, Ozawa T, Sato Y, et al. Posterior mediastinal ganglioneuroblastoma in an adolescent: A case report and review. Thorac Cancer. 2020 Feb;11(2):451–5. https://doi.org/10.1111/1759-7714.13277 PMID:31837198
3. Choi JH, Ro JY. Mediastinal neuroblastoma, ganglioneuroblastoma, and ganglioneuroma: pathology review and diagnostic approach. Semin Diagn Pathol. 2022 Mar;39(2):120–30. https://doi.org/10.1053/j.semdp.2021.06.007 PMID:34167847
4. Badiu Tișa I, Samașca G, Aldea C, Lupan I, Farcau D, Makovicky P. Ganglioneuroblastoma in children. Neurol Sci. 2019 Sep;40(9):1985–9. https://doi.org/10.1007/s10072-019-03932-1 PMID:31147856
5. Pavlus JD, Carter BW, Tolley MD, Keung ES, Khorashadi L, Lichtenberger JP 3rd. Imaging of thoracic neurogenic tumors. AJR Am J Roentgenol. 2016 Sep;207(3):552–61. https://doi.org/10.2214/AJR.16.16018 PMID:27340927
6. Adam A, Hochholzer L. Ganglioneuroblastoma of the posterior mediastinum: a clinicopathologic review of 80 cases. Cancer. 1981 Jan;47(2):373–81. https://doi.org/10.1002/1097-0142(19810115)47:23.0.CO;2-O PMID:7459826
7. Decarolis B, Simon T, Krug B, Leuschner I, Vokuhl C, Kaatsch P, et al. Treatment and outcome of Ganglioneuroma and Ganglioneuroblastoma intermixed. BMC Cancer. 2016 Jul;16(1):542. https://doi.org/10.1186/s12885-016-2513-9 PMID:27465021
8. Mossé YP, Deyell RJ, Berthold F, Nagakawara A, Ambros PF, Monclair T, et al. Neuroblastoma in older children, adolescents and young adults: a report from the International Neuroblastoma Risk Group project. Pediatr Blood Cancer. 2014 Apr;61(4):627–35. https://doi.org/10.1002/pbc.24777 PMID:24038992
9. Fatimi SH, Bawany SA, Ashfaq A. Ganglioneuroblastoma of the posterior mediastinum: a case report. J Med Case Rep. 2011 Jul;5(1):322. https://doi.org/10.1186/1752-1947-5-322 PMID:21781292
10. Molenaar WM, Baker DL, Pleasure D, Lee VM, Trojanowski JQ. The neuroendocrine and neural profiles of neuroblastomas, ganglioneuroblastomas, and ganglioneuromas. Am J Pathol. 1990 Feb;136(2):375–82. PMID:1689542
11. Tobias JD. Anesthetic considerations for endoscopic procedures in children. Semin Pediatr Surg. 1993 Aug;2(3):190–4. PMID:8062040
12. Petrat G, Weyandt D, Klein U. Anesthetic considerations in pediatric laparoscopic and thoracoscopic surgery. Eur J Pediatr Surg. 1999 Oct;9(5):282–5. https://doi.org/10.1055/s-2008-1072263 PMID:10584183
13. McGahren ED, Kern JA, Rodgers BM. Anesthetic techniques for pediatric thoracoscopy. Ann Thorac Surg. 1995 Oct;60(4):927–30. https://doi.org/10.1016/0003-4975(95)00581-5 PMID:7574996

 ORCID
ORCID