Guillermo Adolfo Madrid Díaz1,*, Sergio Andrés Carretero Pardo2, Julián Arturo Barrios Pinzón1, Andrés F. Zuluaga Z.1, Juan Fernando Parada Márquez1
Recibido: 16-04-2024
Aceptado: 12-05-2024
©2025 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 54 Núm. 1 pp. 46-50|https://doi.org/10.25237/revchilanestv54n1-05
PDF|ePub|RIS
Abstract
Recent studies suggest chronic pain is a concern following hysterectomy. New techniques, like intrathecal morphine with general anesthesia, aim to improve pain control. This scoping review explored the impact of intrathecal morphine on post-surgical pain in hysterectomy patients. A literature search (Oct 2023-Dec 2023) identified 5 relevant studies from PubMed, Cochrane Library, and LILACS. These studies showed intrathecal morphine reduced pain scores for up to 72 hours after surgery, decreased opioid use, and improved patient satisfaction. These findings suggest this technique has benefits and warrant a review of current global recommendations for standard anesthetic care in hysterectomy surgery.
Resumen
Estudios recientes indican que el dolor crónico es una preocupación tras la histerectomía. Las técnicas nuevas, como la morfina intratecal con anestesia general, buscan mejorar el control del dolor. Esta revisión exploró el impacto de la morfina intratecal en el dolor posoperatorio en pacientes con histerectomía. Una búsqueda bibliográfica (octubre de 2023-diciembre de 2023) identificó 5 estudios relevantes en PubMed, Cochrane Library y LILACS. Estos estudios mostraron que la morfina intratecal redujo las puntuaciones de dolor hasta 72 h después de la cirugía, disminuyó el uso de opioides y mejoró la satisfacción del paciente. Estos hallazgos sugieren que esta técnica tiene beneficios y justifican una revisión de las recomendaciones globales actuales para la atención anestésica estándar en la cirugía de histerectomía.
-
Introduction
Hysterectomy is the second most common surgery among women of reproductive age[1], with an estimated rate of 350 procedures performed per 100,000 individuals annually[2]. Additionally, it is associated with a high morbidity and mortality burden owing to its inherently painful nature. Approximately 30% of patients undergoing hysterectomy experience severe postoperative pain, while 10% develop chronic pain within the first postoperative year[3].
Inadequately managed postoperative pain is linked to a higher risk of insomnia and depression, which impede proper recovery. Moreover, it increases opioid consumption and the risk of adverse events associated with its chronic use[4]. Furthermore, the physiological implications of pain, characterized by increased cortisol and catecholamine secretion coupled with heightened sympathetic responses, can trigger hypertensive crises and other perioperative complications[5].
Recommendations from the latest update of the Enhanced Recovery After Surgery (ERAS) guidelines for gynecological/on- cological surgery in 2019 present the use of general anesthesia alongside intravenous multimodal analgesia as standard perioperative care. It has been reported that over half of the major gynecological surgeries are performed using this approach[6]. However, postoperative analgesia with this technique is inadequate. Recent studies indicate that up to 22% of patients undergoing hysterectomy continue to experience pelvic pain for up to one year after surgery[7]. Consequently, in response to this challenge, recent scientific evidence has highlighted intrathecal morphine (ITM) as a safe technique when used as an adjunct to general anesthesia, requiring a single injection and offering numerous benefits. These include reduced postoperative pain and opioid consumption, enhanced patient satisfaction with pain control, shorter hospital stays, and improved quality of recovery compared to general anesthesia with intravenous multimodal analgesia[8],[9],[10],[11],[12].
Despite the development of multiple regional anesthesia and analgesia techniques, there is a lack of consensus regarding their use in hysterectomies. The selection of strategies for effective postoperative pain control should be based on the patient’s profile, surgical procedure, and available evidence, presenting a challenge for multidisciplinary collaboration[13]. This scoping review aimed to focus on the evidence concerning the use of intrathecal morphine as an adjunct to general anesthesia in hysterectomies, primarily analyzing its impact on postoperative pain.
-
Methods
Research Question: This scoping review aimed to explore the impact of intrathecal morphine as an adjunct to general anesthesia on postoperative pain in patients undergoing hysterectomy.
Search Strategy: This scoping review followed the PRISMA extended guidelines for Scoping Reviews and employed the SANRA scale for the quality assessment of narrative review articles. Three team members, one medical intern, and two anesthesiologists independently conducted literature searches between October 2023 and December 2023. The databases searched included PubMed, Cochrane Library, and Latin American and Caribbean Health Sciences Literature (LILACS). Search terms included: (intrathecal morphine, hysterectomy) and (morfina intratecal E hysterectomy). English terms were used for searches in PubMed and Cochrane, whereas Spanish terms were used for LILACS.
Inclusion and Exclusion Criteria: Primary studies from all geographical areas, written in English and Spanish, were included. In addition, articles were required to be published in peer-reviewed journals. Studies not written in English or Spanish, those conducted on procedures other than hysterectomy, and those involving intrathecal morphine + the use of spinal local anesthetic were excluded.
Data selection and charting process: Three researchers independently screened the most relevant articles. Initially, duplicates were removed from the search. Subsequently, a secondary analysis based on the inclusion and exclusion criteria led to exclusion of certain articles. Information regarding authors, year of publication, number of patients included, methodology, method of pain measurement, and key outcomes was collected and managed using Excel, as shown in Figure 1.
-
Results
The initial literature search by three researchers independently yielded a total of 31 articles. Following the analysis of duplicate articles and the application of inclusion and exclusion criteria, 5 relevant articles were obtained, as shown in Table 1, focusing on assessing the impact of intrathecal morphine in a blended technique with general anesthesia on postoperative pain in patients undergoing hysterectomy. The data were sourced globally, predominantly from studies conducted in Europe, most of which were published within the last two years.
How does the use of intrathecal morphine as an adjunct to general anesthesia impact postoperative pain?
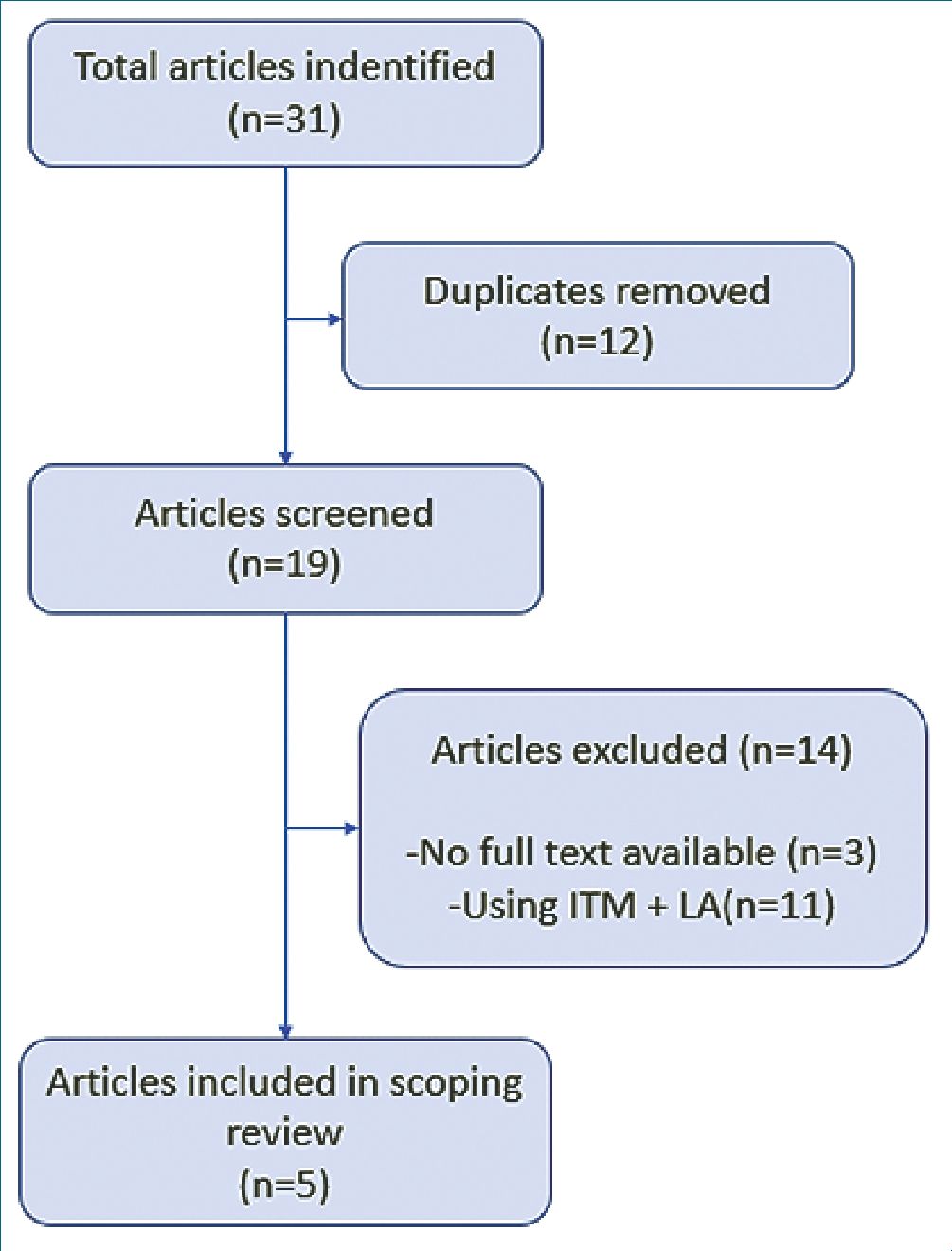
Figure 1. Preferred Reporting Items for Systematic Reviews and Me- ta-Analyses (PRISMA) flow diagram for this scoping review on Intrathecal Morphine for hysterectomy.
-LA (Local anesthetic).
Table 1. Overview of articles relevant about the use of blended technique (GA + ITM without LA) and its impact on postoperative pain in patients undergoing hysterectomy
| Authors (Publication year) | Type study | Type surgery | (n) (#) patients | Pain scale measure | ITM Dose | Results |
| Catarci et al. (2023) | Retrospective cohort | Laparoscopic and mi n i – laparotomy | 644 | NRS | 50, 75 or 100 mcg | Cohort of patients was retrospectively divided into three groups according to the anesthetic management: GA + ITM + LA (Group 1), GA + ITM (Group 2) and GA (Group 3). NRS measured at each visit was lower Groups 1 and 2 in the first 48 hours. |
| Di Filippo et al. (2022) | Case-control | Laparoscopic and laparotomy | 80 | VAS | 125 mcg | ITM patients reported a lower mean VAS in postoperative day 1 (ITM 1.85 ± 1.22 vs PCA 3.16 ± 1.3 p < 0.002) and day 3 (ITM 0.42 ± 0.67 vs PCA 2.56 ± 1.31 p < 0.0001) |
| Jeong Bang et al. (2022) | Clinical trial | Laparotomy | 68 | NRS | 200 mcg | ITM group reported a lower NRS in the first 24 hours postoperative vs sham group p < 0.0001 with a difference in medians of 6 points (95% CI) |
| Rebel et al. (2011) | Retrospective cohort | Vaginal | 121 | VAS | 1,000 mcg | ITM group reported a lower VAS up to 48 hours postoperative (1.2 ± 1.7) vs IVM (4.6 ± 2.8) p < 0.01 |
| Sarma and Boström (1993) | Clinical trial | Laparotomy | 80 | VAS | 0, 100, 300, 500 mcg | ITM patients reported a lower mean VAS up to 20 hours postoperative vs placebo group |
NRS: (Numerical Rating Scale); VAS: (Visual Analogue Scale); mcg: (micrograms); ITM: (intrathecal morphine); GA: (General Anesthesia); IVM: (Intravenous Morphine); CI: (Confidence Interval).
Several articles were excluded from those identified as they involved local anesthetic within the intrathecal morphine mixture. This decision was made as our goal was to assess intrathecal morphine solely for its analgesic properties, not as an anesthetic technique, due to the advantages it presents. The oldest article dates back to 1993[10], while the most recent is from 2023[8]. A total of 993 patients across 5 studies were analyzed, comprising two clinical trials, two retrospective cohorts, and one case-control study.
The Visual Analogue Scale (VAS) and the Numerical Rating Scale (NRS) were the scales used to assess postoperative pain. A wide variety of intrathecal morphine doses were observed in the studies, ranging from low doses of 50 and 100 mcg to high doses of 500 and 1,000 mcg.
All five studies demonstrated that the use of intrathecal morphine in a blended technique with general anesthesia significantly reduced postoperative pain in patients undergoing hysterectomy, irrespective of whether the procedure was performed via laparotomy, laparoscopy, or vaginal approaches. It was noted that pain reduction occurred even within the first 72 postoperative hours[8],[9],[10],[11],12]. Additionally, intrathecal morphine was found to decrease opioid consumption during hospital stay. In the study by Retel et al., it was observed that the group receiving intrathecal morphine received significantly fewer postoperative opioids in the first 24 hours (44.9 ± 35.5 morphine equivalents) compared to the patients in the non-intrathecal morphine group (5.7 ± 8.7 morphine equivalents). Among other outcomes, Jeong’s study revealed that patients receiving intrathecal morphine exhibited significantly higher satisfaction levels with pain control during the initial 48 hours.
-
Discussion
The administration of intrathecal morphine (ITM) was documented in 1900 by Dr. Nicolae Racoviceanu in Romania. However, neuroaxial anesthesia techniques gained popularity in the 1980s, with numerous publications reporting their use in various conditions, particularly chronic oncological pain and obstetrics[14]. ITM has already been proven to be effective in managing severe pain. It is a safe and cost-effective procedure that requires a single injection, providing effective analgesia for the initial 24-72 postoperative hours. Its benefits are so significant that its use has become a standard of care in procedures such as hip arthroplasty, using low doses of 100 pg or less[15].
The objective of applying ITM without a local anesthetic (LA) stem from evidence demonstrating no difference in postoperative pain when using intrathecal local anesthetic versus intrathecal morphine alone. Moreover, by employing this tech nique solely for analgesic purposes using ITM alone, we first avoided sympathetic blockade of the spinal cord, allowing for less hemodynamic instability in patients. Second, early ambulation is facilitated by avoiding motor block. Evidence also reflects better control of postoperative pain when using ITM without LA than when using a combination of ITM and LA[16].
However, the main concern in using ITM is the occurrence of late respiratory depression, a potentially fatal adverse event associated with this intervention. Carvalho et al., published a literature review in 2011 covering the period from 1945 to 2010 with the aim of evaluating this association. Following a review of 195 articles, the incidence of respiratory depression of 0.26% to 3% was estimated using the ITM. Nevertheless, multiple clinical trials analyzed within this literature review using ITM doses in the range of 200-400 mcg reported a 0% incidence of respiratory depression[17]. Similarly, scientific evidence supports the use of low ITM doses of 100 pg or even less, with references reporting a minimum effective dose of 40 pg, demonstrating no analgesic difference with doses of 100 pg[18].
Among the most frequently reported adverse effects of ITM, shivering, itching, and postoperative nausea, and vomiting (PONV) occur in at least 50% of patients receiving ITM. However, these are anticipated adverse effects that are considered minor and easily treatable[19].
The latest update of the Guidelines for Perioperative Care in Gynecologic/Oncology: Enhanced Recovery After Surgery (ERAS) Society recommendations was published in 2019. This update mentions the standard of care for the anesthetic protocol as the use of general anesthesia, either balanced with inhalation anesthesia or total intravenous anesthesia, combined with intravenous multimodal analgesia. It does not extensively address regional anesthesia techniques or their benefits in controlling postoperative pain; thus, it does not recommend their use[6]. This might be due to recent studies demonstrating the benefits of ITM in a blended technique with general anesthesia in the years 2022 and 2023.
-
Conclusions
Hysterectomy is a major surgery frequently performed worldwide and is associated with significant postoperative pain and a high risk of chronic pain when not adequately controlled. ITM is a rapid, safe, and cost-effective procedure, with evidence demonstrating its benefits in terms of pain control, functionality, and patient satisfaction. However, further studies are needed to expand the current literature and evidence because of the scarcity of references. Nonetheless, based on this scoping review, the benefits of this technique are evident, suggesting a review of the existing worldwide recommendations regarding the standard anesthetic care provided to patients undergoing hysterectomy through any surgical approach.
-
References
1. Carpi CA, Neto AG, Gusmão RA, Silva TA, Gomez MV, Castro-Junior CJ. Intrathecal Morphine Versus Ketamine in Postoperative Pain After Hysterectomy: Double-Blinded, Randomized Clinical Trial. J Perianesth Nurs. 2020 Dec;35(6):580–585.e2. https://doi.org/10.1016/j.jopan.2020.06.013 PMID:32855054
2. Lycke KD, Kahlert J, Damgaard R, Mogensen O, Hammer A. Trends in Hysterectomy Incidence Rates During 2000-2015 in Denmark: Shifting from Abdominal to Minimally Invasive Surgical Procedures. Clin Epidemiol. 2021 Jun;13:407–16. https://doi.org/10.2147/CLEP.S300394 PMID:34103999
3. Liu Y, Xiao S, Yang H, Lv X, Hou A, Ma Y, et al.; CAPOPS Group. Postoperative pain-related outcomes and perioperative pain management in China: a population-based study. Lancet Reg Health West Pac. 2023 Jun;39:100822. https://doi.org/10.1016/j.lanwpc.2023.100822 PMID:37927993
4. Carr EC. Exploring the effect of postoperative pain on patient outcomes following surgery. Acute Pain. 2000;3(4):183–93. https://doi.org/10.1016/S1366-0071(00)90003-2.
5. Wu CL, Rowlingson AJ, Partin AW, Kalish MA, Courpas GE, Walsh PC, et al. Correlation of postoperative pain to quality of recovery in the immediate postoperative period. Reg Anesth Pain Med. 2005;30(6):516–22. https://doi.org/10.1097/00115550-200511000-00003 PMID:16326335
6. Nelson G, Bakkum-Gamez J, Kalogera E, Glaser G, Altman A, Meyer LA, et al. Guidelines for perioperative care in gynecologic/oncology: Enhanced Recovery After Surgery (ERAS) Society recommendations-2019 update. Int J Gynecol Cancer. 2019 May;29(4):651–68. https://doi.org/10.1136/ijgc-2019-000356 PMID:30877144
7. Grundström H, Fredrikson M, Alehagen S, Berterö C, Kjølhede P. Incidence of self-reported pelvic pain and risk factors for pain 1 year after benign hysterectomy: A register study from the Swedish National Quality Registry for Gynecological Surgery. Acta Obstet Gynecol Scand. 2023 Oct;102(10):1359–70. https://doi.org/10.1111/aogs.14455 PMID:36073635
8. Bang YJ, Lee EK, Kim CS, Hahm TS, Jeong H, Cho YJ, et al. The Effect of Intrathecal Morphine on Postoperative Opioid Consumption in Patients Undergoing Abdominal Surgery for Gynecologic Malignancy: A Randomized Sham-Controlled Trial. Anesth Analg. 2023 Sep;137(3):525–33. https://doi.org/10.1213/ANE.0000000000006358 PMID:36727850
9. Catarci S, Zanfini BA, Capone E, Vassalli F, Frassanito L, Biancone M, et al. Blended (Combined Spinal and General) vs. General Anesthesia for Abdominal Hysterectomy: A Retrospective Study. J Clin Med. 2023 Jul;12(14):4775. https://doi.org/10.3390/jcm12144775 PMID:37510890
10. Sarma VJ, Boström UV. Intrathecal morphine for the relief of post-hysterectomy pain—a double-blind, dose-response study. Acta Anaesthesiol Scand. 1993 Feb;37(2):223–7. https://doi.org/10.1111/j.1399-6576.1993.tb03705.x PMID:8447215
11. DI Filippo A, Capezzuoli T, Fambrini M, Cariti G, Orlandi G, Vannucci G, et al. Enhanced recovery after gynecological surgery: comparison between intrathecal and intravenous morphine multimodal analgesia. Minerva Obstet Gynecol. 2023 Apr;75(2):145–9. https://doi.org/10.23736/S2724-606X.21.04961-7 PMID:34851074
12. Rebel A, Sloan P, Andrykowski M. Retrospective analysis of high-dose intrathecal morphine for analgesia after pelvic surgery. Pain Res Manag. 2011;16(1):19–26. https://doi.org/10.1155/2011/691712 PMID:21369537
13. Coccolini F, Corradi F, Sartelli M, Coimbra R, Kryvoruchko IA, Leppaniemi A, et al. Postoperative pain management in non-traumatic emergency general surgery: WSES-GAIS-SIAARTI-AAST guidelines. World J Emerg Surg. 2022 Sep;17(1):50. https://doi.org/10.1186/s13017-022-00455-7 PMID:36131311
14. Kissin I. Clinical studies that initiated the use of spinal opioids for the treatment of pain: A new approach to historical review. Curr Rev Clin Exp Pharmacol. 2023;19(1):61–7. https://doi.org/10.2174/2772432817666220609093243 PMID:35692145
15. Rojas A, Hernández M, Vidal P, Balkenhol M, Opazo M, Riquelme M. Low dose intrathecal morphine for hip arthroplasty. Rev Chil Anest. 2020;49(4):153–60. https://doi.org/10.25237/revchilanestv49n04-11.
16. Meylan N, Elia N, Lysakowski C, Tramèr MR. Benefit and risk of intrathecal morphine without local anaesthetic in patients undergoing major surgery: meta-analysis of randomized trials. Br J Anaesth. 2009 Feb;102(2):156–67. https://doi.org/10.1093/bja/aen368 PMID:19151046
17. Sultan P, Gutierrez MC, Carvalho B. Neuraxial morphine and respiratory depression: finding the right balance. Drugs. 2011 Oct;71(14):1807–19. https://doi.org/10.2165/11596250-000000000-00000 PMID:21942973
18. Yamaguchi H, Watanabe S, Fukuda T, Takahashi H, Motokawa K, Ishizawa Y. Minimal effective dose of intrathecal morphine for pain relief following transabdominal hysterectomy. Anesth Analg. 1989 Apr;68(4):537–40. https://doi.org/10.1213/00000539-198904000-00023 PMID:2929987
19. Grape S, El-Boghdadly K, Albrecht E. Management of adverse effects of intrathecal opioids in acute pain. Best Pract Res Clin Anaesthesiol. 2023 Jun;37(2):199–207. https://doi.org/10.1016/j.bpa.2023.02.002 PMID:37321767

 ORCID
ORCID