Sarah Bastawy I. Ph.D*, Kelani Abdelsalam1, Ragaa Ahmed Herdan1, Rasha Ahmed Ali Hamed1
Recibido: 18-01-2025
Aceptado: 27-02-2025
©2025 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 54 Núm. 6 pp. 865-870|https://doi.org/10.25237/revchilanestv54n6-12
PDF|ePub|RIS
Bloqueo epidural versus cuadrado lumbar para analgesia posoperatoria en ne- frectomías abiertas en adultos: un ensayo controlado, aleatorizado, doble ciego
Abstract
Background: An epidural is not a suitable technique for all patients and is contraindicated in patients with local infection and previous spine surgery, while Quadratus lumborum block (QLB) has been introduced recently as a component of multimodal analgesia for thoracic and abdominal surgeries. The aim of this work was to compare the analgesic effect of epidural block versus ultrasound guided quadratus lumborum in radical nephrectomy. Methods: This prospective randomized, double-blinded clinical trial was carried out on 70 patients aged from 20 to 60 years old, both sexes, American Society of Anaesthesiologists I and II physical status, scheduled for open nephrectomies. Patients were divided into two equal groups: Group QLB: received ultrasound guided QLB type 3 with a single shot of 30 ml of bupivacaine 0.25% before induction of GA (0.2-0.4 ml/kg) on each side and Group epidural block (EB): received epidural block followed by general anaesthesia (GA). Patients were given 30 ml of bupivacaine 0.25% for analgesia. Results: Visual analogue scale (VAS) throughout the whole postoperative observation period was significantly different between the studied groups. The reduction in pain score was significantly higher in the QLB group as indicated by the interaction analysis (P < 0.002). EB group had significantly longer analgesia duration than QLB group (P = 0.005). EB group required lower opioid than QLB group during first postoperative day. Conclusions: QLB is less effective than epidural block in controlling postoperative pain after radical nephrectomy. Pain scores in the first 24 hours were significantly lower in the epidural group.
Resumen
Antecedentes: La epidural no es una técnica adecuada para todos los pacientes y está contraindicada en pacientes con infección local y cirugía de columna previa, mientras que el bloqueo del cuadrado lumbar (QLB) se ha introducido recientemente como componente de la analgesia multimodal para cirugías torácicas y abdominales. El objetivo de este trabajo fue comparar el efecto analgésico del bloqueo epidural versus el cuadrado lumbar guiado por ecografía en la nefrectomía radical. Métodos: Este ensayo clínico prospectivo, aleatorizado, doble ciego, se realizó en 70 pacientes con edades de 20 a 60 años, ambos sexos, estado físico de la Sociedad Americana de Anestesiólogos I y II, programados para nefrectomía abierta. Los pacientes se dividieron en dos grupos iguales: Grupo QLB: recibió QLB tipo 3 guiado por ultrasonido con una única inyección de 30 ml de bupivacaína al 0,25% antes de la inducción de GA (0,2-0,4 ml/kg) en cada lado y Grupo bloqueo epidural (EB): recibió bloqueo epidural seguido de anestesia general (GA). Los pacientes recibieron 30 ml de bupivacaína al 0,25% como analgesia. Resultados: La escala visual analógica (EVA) durante todo el período de observación postoperatoria fue significativamente diferente entre los grupos estudiados. La reducción en la puntuación del dolor fue significativamente mayor en el grupo QLB como lo indica el análisis de interacción (P < 0,002). El grupo EB tuvo una duración de la analgesia significativamente mayor que el grupo QLB (P = 0,005). El grupo EB requirió menos opioides que el grupo QLB durante el primer día posoperatorio. Conclusiones: QLB es menos eficaz que el bloqueo epidural en el control del dolor posoperatorio tras nefrectomía radical. Las puntuaciones de dolor en las primeras 24 h fueron significativamente más bajas en el grupo epidural.
-
Introduction
Abdominal surgeries are usually associated with significant postoperative pain. Postoperative analgesia following abdominal surgeries is essential to allow effective coughing, early mobilization, and to reduce the incidence of postoperative respiratory complications[1],[2].
Administration of systemic analgesia after abdominal surgeries may be precluded by impaired renal function and respiratory complications from the use of opioids[3].
Other techniques include intramuscular or intravenous injection of paracetamol or non-steroidal anti-inflammatory drugs. However, none of these methods were proven to be highly effective[4].
Regional anaesthesia may reduce the rate of chronic pain after surgery. Thoracic epidural blockade (TEB) using local anaesthetic agents has been widely regarded as the gold standard for analgesia and reduction of associated complications following abdominal surgery including open nephrectomy, however, it has unfavourable side effects such as paraesthesia, hypotension, hematomas, an impaired motor of lower limbs and urinary retention that could delay recovery[5].
The risks associated with insertion of the epidural catheter include accidental Dural puncture, inadvertent high block, local anaesthetic toxicity and total spinal anaesthesia (inadvertent spinal injection of an epidural dose of local anaesthetic). Nerve injury, epidural hematoma and abscess are rare but serious complications[6]. Thoracic epidural blocks nerves bilaterally, and sympathetic nerve block can result in hypotension due to both vasodilatation and cardiac depression. This requires cautious fluid administration in order to avoid fluid overload in susceptible patients[7].
An epidural is not a suitable technique for all patients and is contraindicated in patients with local infection, previous spine surgery, disorders of blood clotting and in those taking anticoagulant and anti-platelet therapy[8].
Quadratus lumborum muscle is a paired muscle of the left and right posterior abdominal wall, it is the deepest abdominal muscle and commonly referred to as a back muscle. Each is irregular and quadrilateral in shape[9].
Quadratus lumborum block (QLB) has been introduced recently as a component of multimodal analgesia for thoracic and abdominal surgeries as: caesarean section (CS), hip arthroplasty, inguinal hernia repair and nephrectomise[10]. Our hypothesis was that performing ultrasound guided QLB was more superior or equal to epidural block in providing postoperative analgesia for patients undergoing open nephrectomy under general anaesthesia (GA). The aim of this study was to compare the analgesic effect of epidural block versus ultrasound guided quadratus lumborum in radical nephrectomy.
-
Patients and Methods
This prospective randomized, double-blinded clinical trial was carried out on 70 patients aged from 20 to 60 years old, both sexes, American Society of Anaesthesiologists (ASA) class I or II physical status, scheduled for open nephrectomies. The study was done after approval from the Ethical Committee Assiut University Hospitals, Assiut, Egypt. (Approval code: 17101594) and registration of clinicaltrials.gov (ID: NCT05174364). An informed written consent was obtained from the patients.
Exclusion criteria were significant organ dysfunctions (e.g., cardiac, respiratory, renal, or liver disorders), morbid obesity (body mass index (BMI) > 40), patient with known hypersensitivity to amide local anaesthetics, patient with any contraindication for intrathecal anaesthesia such as coagulopathy, psychiatric disorders, which could make observational pain intensity assessment difficult, pregnancy and skin lesions or wounds at the puncture site of the proposed block.
-
Randomisation and blinding
Using a computer-generated randomization, patients were randomly allocated into two equal groups: Group QLB (comparative group): received ultrasound guided QLB type 3 with a single shot of 30 ml of bupivacaine 0.25% before induction of GA (0.2-0.4 ml/kg) on each side. Group EB (control group): received epidural block followed by GA. Patients were given 30 ml of bupivacaine 0.25% for analgesia. The trial was planned that neither the investigators to collect data nor the patients or even the surgeon were aware of the group allocation, block approach, drugs received, patient monitoring or data collection.
-
Intraoperative management
An intravenous cannula 18G were inserted in the dorsum of the non-dominant hand for IV drugs, fluids, and emergency situations. After intravenous access securing, infusion of normal saline 0.9% solution 4 ml/kg/h was started followed by standard fluid maintenance therapy according to the patient’s weight. Intraoperative monitoring included electrocardiogram (ECG), pulse oximetry, non-invasive blood pressure, capnography, and temperature probe. Hemodynamics including heart rate (HR), mean blood pressure (MBP) and peripheral oxygen saturation (SpO2) were recorded before block, after the block, after induction of aesthesia, and every 20 minutes till the end of surgery. GA was standardized for all patients in both groups after 3 minutes of 100% oxygen via face mask using Fentanyl 1 mcg/kg, propofol 2 mg/kg and atracurium 0.5 mg/kg. Cuffed endotracheal intubation with appropriate size to the patient’s age was inserted under direct laryngoscopy after complete muscular relaxation. The endotracheal tube then was secured at the appropriate length, by adhesive tape at the angle of the mouth. Controlled mechanical ventilation was used to maintain end tidal CO2 at 35 ± 5 mmHg. GA was maintained with 2-3 MAC sevoflurane delivered in 100% O2. All patients were continuously monitored intraoperatively for any episodes of hypotension or bradycardia.
-
Technique of epidural block
Epidural block for the control group was done before induction of GA. Patients were positioned in the sitting position, an 18-gauge Tuohy needle was inserted into epidural space of L1-2 intervertebral space under complete aseptic condition. In the medial approach, the site of insertion of the needle was between the spaces created by the vertebral spinous processes. Upon locating the desired spot, lidocaine 1% was injected into the skin and underlying tissues to decrease the discomfort with the advancement of the epidural needle. Once achieving local anaesthesia, the epidural needle was advanced with its stylet in place and with its bevel point cephalad. The epidural needle was advanced through the skin, subcutaneous tissue, supraspinous, and interspinous ligaments. The needle was advanced while applying pressure to the plunger. Once the ligamentum flavum was pierced, a loss in resistance was noted; this was the epidural space, and 5-10 cc of saline was injected to expand the epidural space; this decreased the risk of vascular injury. Before the first surgical incision, bupivacaine 0.25% 30 ml was administered epidurally.
-
Technique of quadratus lumborum block
Bilateral QL block type 3 (anterior) for the intervention group was performed on both sides of the patient before induction of GA. Patient was positioned in semi-lateral decubitus and by low frequency ultrasonography (USG) guidance attached to inferior lumbar region (Petit’s triangle) that was consisted of inferior iliac crest and bordered by two muscles such as latissimus dorsi muscle in the posterior, abdominal external oblique muscle in the anterior. The ultrasound guide displayed the Shamrock sign, where the transverse process of vertebrae L4 rolled as the trunk, erector spinae muscle on the posterior side, psoas major (PM) on the anterior side, and QL muscle on the lateral side. After the visualization of QL and PM muscles, the Conti plex R needle was directed parallel to the posterior side of the ultrasound probe until the tip of needle was confirmed in the border of QL and PM muscle. The aspiration test revealed a negative result, and then 1 mL of NaCl 0.9% was injected to get the sign of hydro dissection. 30 mL of bupivacaine 0.25% was injected into the fascia between PM and QL muscles on each side. After completion of the surgical procedure, sevoflurane was discontinued; residual neuromuscular blocking agents were pharmacologically reversed with the standard reversal doses of neostigmine bromide 0.04 mg/kg in atropine sulphate 0.02 mg/kg. The patients then were ventilated by 100% oxygen till full consciousness regained and the patients started following verbal commands. At that point endotracheal tubes were removed after gentle suction of secretions through the tube and the oropharyngeal cavity.
The primary outcome was to compare the effectiveness of bilateral QLB and epidural analgesia for postoperative pain management using visual analogy scale (VAS) measured in post anaesthesia care unit (PACU) until 24 hours after surgery in patients undergoing elective open nephrectomies under GA. The secondary outcomes were the first time to rescue analgesia (duration from end of anaesthesia until first attempt of nalbuphine requirement in minutes in the dose of 0.1 mg/kg nalbuphine) and total amount of opioid consumption that was recorded throughout the first postoperative day, intraoperative and postoperative hemodynamic variables (heart rate, mean blood pressure, peripheral oxygen saturation and end tidal CO2), any complications as postoperative nausea and vomiting (PONV) and headache, duration of PACU stay and postoperative duration of hospitalization and patients’ satisfaction.
-
Sample size calculation
Using G* Power 3 software[11]. Depending on the results of an earlier study[12], a calculated minimum sample of 62 adults having open partial nephrectomies were needed. The sample was increased to include 70 patients to compensate the possible dropouts. Patients were divided into two equal groups (Group EB (n = 35); received epidural block, and group QLB (n = 35) received QLB to detect an effect size of 0.42 in the mean pain scores with an error probability of 0.05 and 80% power on a one tailed test.
-
Statistical analysis
Statistical analysis was done by SPSS v26 (IBM Inc., Chicago, IL, USA). Quantitative variables were presented as mean and standard deviation (SD) and compared between the two groups utilizing unpaired Student’s t-test. Qualitative variables were presented as frequency and percentage (%) and analysed using the Chi-square or Fisher’s exact test when appropriate. A two-tailed P value < 0.05 was considered statistically significant.
-
Results
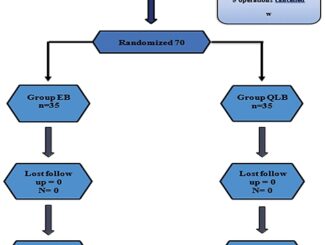
In this study, 82 patients were assessed for eligibility, 12 patients did not meet the criteria and 7 patients refused to participate in the study. The remaining 70 patients were randomly allocated into two equal groups (35 patients in each). All allocated patients were followed-up and analysed statistically (Figure 1).
Demographic data, ASA status and surgery duration were insignificant between the studied groups Table 1. MAP and HR were significantly lower in the epidural group than QLB group (Figure 2). However, the differences were clinically insignificant as it still within the normal ranges. VAS scores were significantly lower in the epidural group than the QLB group through out the first 24 h postoperative (P < 0.05) Figure 3 and Table 2.
Likewise, EB group had significantly (P = 0.005) longer analgesia time denoted by delayed 1 st analgesia request (6 ± 1.3 hours) than QLB group (4 ± 1.5 hours). Also, EB group had significantly (P=0.043) lower opioid consumption (8 ± 2.7 mg) than QLB group (13 ± 3 mg) during first postoperative day.
There was insignificant difference between the studied groups regarding incidence of PONV one cases complained of PONV in QLB versus 2 cases in epidural group (P = 0.5). Significant lower rate of headache recorded in the QLB group versus the epidural group (0% vs 5.7%, P = 0.03 respectively) Table 3.
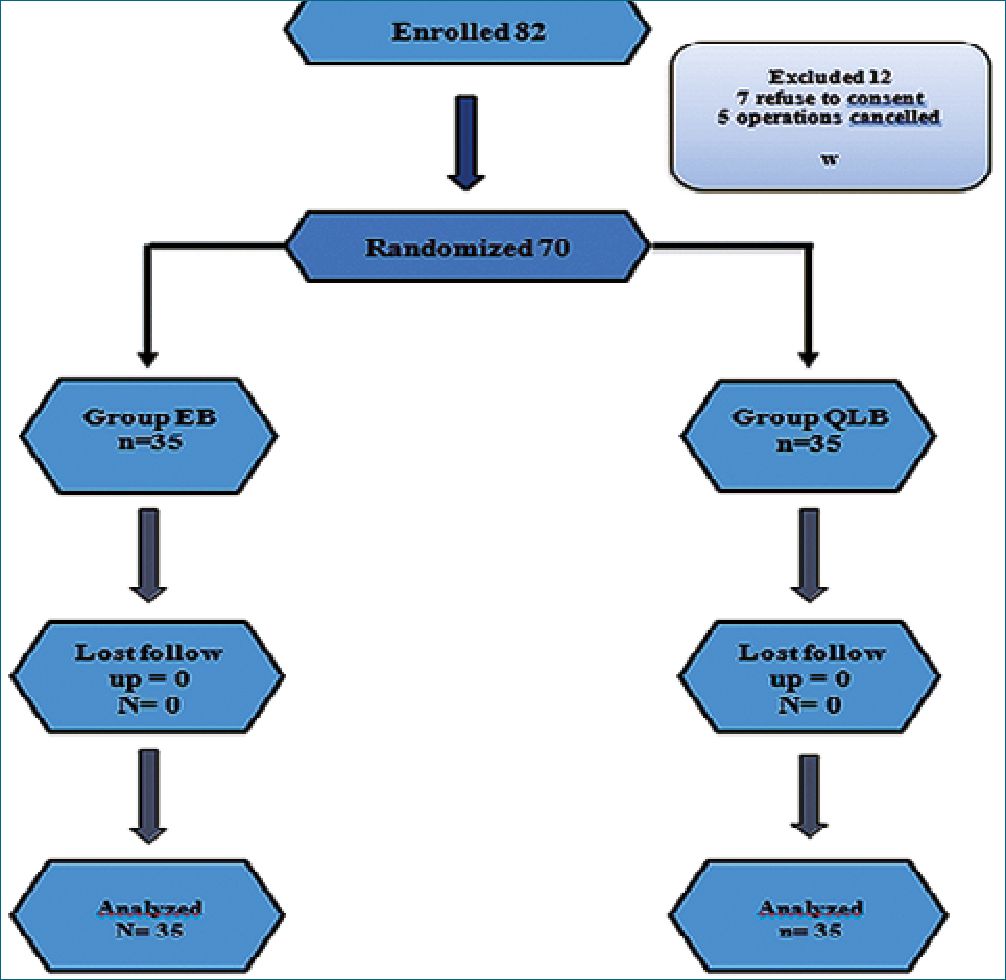
Figure 1. Consort flow chart of the studied groups.
Figure 2. Mean (A) heart rate and; (B) mean arterial blood pressure.
Table 1. Demographic data and ASA status of the studied groups
| EB Group (n = 35) | QLB Group (n = 35) | P | ||
| Age/years | 43.74 ± 11.1 | 41.43 ± 11.4 | NS | |
| Sex | Male | 24 (68.6%) | 25 (71.4%) | NS |
| Female | 11 (31.4%) | 10 (28.6%) | ||
| Weight/kg | 71.66 ± 12.3 | 73.20 ± 8.4 | NS | |
| Height (cm) | 165.49 ± 6.8 | 165.66 ± 7.9 | NS | |
| BMI | 26.14 ± 4.2 | 26.66 ± 3.7 | NS | |
| ASA | I | 30 (65.7%) | 32 (91.4%) | NS |
| II | 5 (34.3%) | 3 (8.6%) | ||
| Surgery duration | 167 ± 7 | 170± | NS |
Data are presented as mean ± SD or frequency (%); EB: Epidermolysis bullosa; QLB: Quadratus lumborum block; BMI: Body mass index; ASA: American society of anesthesiologists.
-
Discussion
US-guided truncal fascial plane blocks have gained popularity for postoperative pain control in several types of abdominal surgeries. One of the most promising is QLB, which is thought to also relieve visceral pain. Three distinct types of QLBs have been described (lateral, posterior, and anterior)[13].
Results were inconsistent with our hypothesis that quadra- tus lumborum block is non inferior to epidural block in postoperative analgesia. Pain scores in the first 24 hours were significantly lower in the epidural group. Furthermore; 24-hour opioid consumption was significantly lower in the epidural group. Our results were in consistent with Elsharkawy et al.[14], who found that epidural block is superior to quadrates lumborum in controlling postoperative pain and reducing postoperative opioid use after open nephrectomy.
In contrast to our results, an earlier trial compared epidural and quadrates lumborum in laparoscopic nephrectomy, the authors concluded that quadrates lumborum is as effective as epidural block in controlling postoperative pain and reducing analgesic consumption after laparoscopic nephrectomy. However, difference in the results could be explained by more pain and manipulation associated with open surgery than laparoscopic surgery[12].
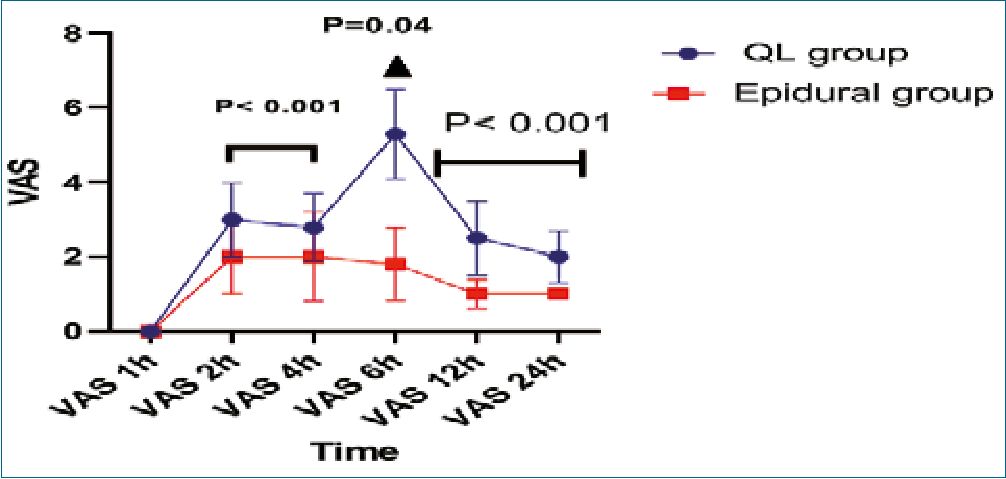
Figure 3. Mean VAS score Comparisons between Groups over Time.
Table 2. Comparison of mean VAS score between groups over time
| EB Group (n = 35) | QLB Group (n = 35) | P | ||
| VAS score | 1-h | 0 | 0 | N. S |
| 2-h | 2.1± 1.1 | 3.1 ± 1.1 | < 0.001* | |
| 4-h | 2.1 ± 1.2 | 2.8 ± 0.9 | < 0.04* | |
| 6-h | 1.8 ± 1.1 | 3.6 ± 1.2 | < 0.001* | |
| 12-h | 1.1 ± 0.4 | 2.5 ± 1.1 | < 0.001* | |
| 24-h | 1.1 ± 0.1 | 2.1 ± 0.7 | < 0.001* | |
| P-value** | < 0.001* | < 0.001* | P = 0.002# | |
Data are presented as mean ± SD; * significant p value < 0.05; *Between groups; **Within Group; #: interaction between group and time; VAS: visual analogue scale; EB: Epidural block; QLB: Quadratus lumborum block.
Table 3. Postoperative data
| EB group | QLB | P- value | |
| Analgesia time | 4 ± 1.5 | 6 ± 1.3 | 0.005 |
| 24h opioid consumption | 13 ± 3 | 8 ± 2.7 | < 0.001 |
| PONV | 1 (2.9%) | 2 (5.7%) | 0.5 |
| Headache | 0 (0%) | 5 (14.3%) | 0.03 |
However, several earlier studies were in contrast to the result of the current study, but none of them compared the two blocks in such a high anatomical intervention as nephrectomy in adults. Öksüz et al.[15], compared the effect of posterior QLB and continuous EB in paediatric patients undergoing inguinal hernia repair and orchiopexy, QLB patients had lower pain scores, required less rescue analgesia, and had more satisfied parents. Ahmad et al.[16], concluded that Quadratus lamborum block is superior to epidural block in providing perioperative analgesia to paediatric patients safely and effectively. In addition, it provides more stable intraoperative hemodynamics, less need for intraoperative narcotics, lower postoperative pain scores, less need for rescue analgesia, and greater parental satisfaction in comparison to continuous EB[14]. Korgvee et al.[17], found no difference in the amount of consumed postoperative analgesia between both groups, but epidural analgesia was associated with more hemodynamic instability in perioperative period. Lin et al.[18], suggested that analgesic efficacy of QLB could be explained by blockade of the sympathetic fibres and visceral fibres in the thoracolumbar fascia. According to the cadaveric reports, each approach of QLB has a different mechanism of action. In QLB1 or QLB2, the injected local anaesthetics are reportedly confined to the thoracolumbar fascia or transversus abdominis plane (TAP). In QLB3, the injected local anaesthetics may spread to the mid to lower thoracic paravertebral space and the lumbar nerve roots. The three-dimensional computed tomography images of patients have revealed that QLB1 spread in the TAP, QLB2 spread in the TAP and posterior region of the quadratus lumborum muscle, and transverse oblique paramedian QLB3 spread to the lumbar and thoracic paravertebral regions. Tamura et al.[19], reported that in magnetic resonance imaging, QLB2 appeared to have a wider dye spread compared to QLB1. Furthermore, QLB3 is a deep approach, which is reported to result in a greater motor blockade and the risk of needle trauma of the pleura and kidney. Consequently, in clinical practice, a higher number of people select QLB2. One small sample-size study reported that the analgesic effect of QLB3 was a superior to that of QLB2 in caesarean delivery. However, Brixel et al.[20], recently reported that 30 mL of the QLB2 solution could reach multiple locations around the quadratus lumborum muscle when sonographic
localization was used. Limitations of this study including that the sample size was relatively small. The study was in a single centre.
-
Conclusions
Results were inconsistent with our hypothesis that Quadrates lumborum block is non inferior to epidural block in postoperative analgesia. Pain scores in the first 24 hours were significantly lower in the epidural group, furthermore; 24-hour opioid consumption was significantly lower in the epidural group.
Financial support and sponsorship Nil.
Conflict of Interest Nil.
-
References
1. Kararmaz A, Kaya S, Karaman H, Turhanoglu S, Ozyilmaz MA. Intraoperative intravenous ketamine in combination with epidural analgesia: postoperative analgesia after renal surgery. Anesth Analg. 2003 Oct;97(4):1092–6. https://doi.org/10.1213/01.ANE.0000080205.24285.36 PMID:14500163
2. Shoeibi G, Babakhani B, Mohammadi SS. The efficacy of ilioinguinal-iliohypogastric and intercostal nerve co-blockade for postoperative pain relief in kidney recipients. Anesth Analg. 2009 Jan;108(1):330–3. https://doi.org/10.1213/ane.0b013e31818c1b13 PMID:19095869
3. Ghods AJ, Mahdavi M. Organ transplantation in Iran. Saudi J Kidney Dis Transpl. 2007 Nov;18(4):648–55. PMID:17951961
4. Lönnqvist PA, Olsson GL. Paravertebral vs epidural block in children. Effects on postoperative morphine requirement after renal surgery. Acta Anaesthesiol Scand. 1994 May;38(4):346–9. https://doi.org/10.1111/j.1399-6576.1994.tb03905.x PMID:8067221
5. Andreae MH, Andreae DA. Local anaesthetics and regional anaesthesia for preventing chronic pain after surgery. Cochrane Database Syst Rev. 2012 Oct;10:CD007105. https://doi.org/10.1002/14651858.CD007105.pub2 PMID:23076930
6. De Cosmo G, Aceto P, Gualtieri E, Congedo E. Analgesia in thoracic surgery: review [review]. Minerva Anestesiol. 2009 Jun;75(6):393–400. PMID:18953284
7. Carver A, Wou F, Pawa A. Do outcomes differ between thoracic epidurals and continuous fascial plane blocks in adults undergoing major abdominal surgery? Curr Anesthesiol Rep. 2024;14(1):25–41. https://doi.org/10.1007/s40140-023-00594-w.
8. Davies RG, Myles PS, Graham JM. A comparison of the analgesic efficacy and side-effects of paravertebral vs epidural blockade for thoracotomy—a systematic review and meta-analysis of randomized trials. Br J Anaesth. 2006 Apr;96(4):418–26. https://doi.org/10.1093/bja/ael020 PMID:16476698
9. Jairakdee Y, Chansirinukor W, Sitti T. Effect of releasing quadratus lumborum muscle on hip and knee muscle length in asymptomatic individuals. J Bodyw Mov Ther. 2021 Apr;26:542–7. https://doi.org/10.1016/j.jbmt.2020.11.008 PMID:33992295
10. Wang J, Chu T, Sun R, Xu A. Analgesic efficacy of quadratus lumborum block in patients undergoing nephrectomy: A systematic review and meta-analysis. Pain Med. 2023 May;24(5):476–87. https://doi.org/10.1093/pm/pnac166 PMID:36321993
11. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007 May;39(2):175–91. https://doi.org/10.3758/BF03193146 PMID:17695343
12. Yadav M, Agrawal M, Bansal P, Prateek MK, Garg MK, Yadav A. Ultrasound-guided quadratus lumborum block versus ilioinguinal-iliohypogastric nerve block with wound infiltration for postoperative analgesia in unilateral inguinal surgeries: A randomised controlled trial. Indian J Anaesth. 2023 Mar;67(3):302–6. https://doi.org/10.4103/ija.ija_578_22 PMID:37250519
13. Aditianingsih D, Pryambodho, Anasy N, Tantri AR, Mochtar CA. A randomized controlled trial on analgesic effect of repeated Quadratus Lumborum block versus continuous epidural analgesia following laparoscopic nephrectomy. BMC Anesthesiol. 2019 Dec;19(1):221–4. https://doi.org/10.1186/s12871-019-0891-7 PMID:31805855
14. Elsharkawy H, El-Boghdadly K, Barrington M. Quadratus lumborum block: anatomical concepts, mechanisms, and techniques. Anesthesiology. 2019 Feb;130(2):322–35. https://doi.org/10.1097/ALN.0000000000002524 PMID:30688787
15. Öksüz G, Arslan M, Urfalıoğlu A, Güler AG, Tekşen Ş, Bilal B, et al. Comparison of quadratus lumborum block and caudal block for postoperative analgesia in pediatric patients undergoing inguinal hernia repair and orchiopexy surgeries: a randomized controlled trial. Reg Anesth Pain Med. 2020 Mar;45(3):187–91. https://doi.org/10.1136/rapm-2019-101027 PMID:31907294
16. Ahmad AH, Kasem AA, Tolba MA. Posterior quadratus lumborum versus caudal epidural block for perioperative analgesia in pediatric patients undergoing upper abdominal surgeries: Arandomized, double-blind trial. Egypt J Anaesth. 2024;40(1):24–33. https://doi.org/10.1080/11101849.2023.2297327.
17. Korgvee A, Veskimae E, Huhtala H, Koskinen H, Tammela T, Junttila E, et al. Posterior quadratus lumborum block versus epidural analgesia for postoperative pain management after open radical cystectomy: A randomized clinical trial. Acta Anaesthesiol Scand. 2023 Mar;67(3):347–55. https://doi.org/10.1111/aas.14188 PMID:36547262
18. Lin C, Wang X, Qin C, Liu J. Ultrasound-guided posterior quadratus lumborum block for acute postoperative analgesia in adult patients: A meta-analysis of randomized controlled trials. Ther Clin Risk Manag. 2022 Mar;18:299–313. https://doi.org/10.2147/TCRM.S349494 PMID:35378766
19. Tamura T, Yokota S, Ando M, Kubo Y, Nishiwaki K. A triple-blinded randomized trial comparing spinal morphine with posterior quadratus lumborum block after cesarean section. Int J Obstet Anesth. 2019 Nov;40:32–8. https://doi.org/10.1016/j.ijoa.2019.06.008 PMID:31353177
20. Brixel SM, Biboulet P, Swisser F, Choquet O, Aarab Y, Nguyen H, et al. Posterior quadratus lumborum block in total hip arthroplasty: A randomized controlled trial. Anesthesiology. 2021 May;134(5):722–33. https://doi.org/10.1097/ALN.0000000000003745 PMID:33740816

 ORCID
ORCID