Matías David Ontivero MD. 1 , José Luis Campos MD. 2 , María Hernández MD. 3 , Julio Lapalma MD. 4
Recibido: 16-09-2021
Aceptado: 02-11-2021
©2022 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 51 Núm. 5 pp. 586-592|https://doi.org/10.25237/revchilanestv5126071037
PDF|ePub|RIS
Estudio observacional prospectivo: eficacia analgésica del bloqueo erector de espina versus bloqueo del cuadrado posterior en cirugía pediátrica ambulatoria
Abstract
Study Objective: Our hypothesis is that ESP block is equal or superior in providing analgesia than the posterior QL block in abdominal surgery in ambulatory surgery. Design: Prospective observational study comparing the analgesic efficacy of ESP block and QLII block for abdominal surgery in pediatrics. Patients: A total of 20 patients undergoing ambulatory abdominal surgery (urology and general surgery), ASAI-II, age between 6 months and 14years old within March-April 2018, under general anesthesia were included. All participants were randomized to receive an erector spinae or quadratus lumborum block prior to the procedure. Measurements: Perioperative opioid consumption, use of non-opiate analgesia and pain scores were measured. Intraoperative hemodynamics (blood pressure and heart rate and pulse oximetry) as well as presence of adverse events or postoperative complications (nausea or vomiting, respiratory depression and sedation) were documented. Main Results: In both groups the majority of patients reported mild or no pain in the first 24hs with no pain after 24 h. Only 3 patients (15%) in the ESP group and 2 (10%) in the QLII group required rescue analgesia postoperatively. Hemodynamic stability was maintained in both groups. No complications were reported. Conclusions: This study supports the analgesic efficacy and hemodynamic stability with ESP and QL blocks in the ambulatory setting in children. The superficiality of the needle end point in both techniques makes them a safe alternative in pediatrics.
Resumen
Objetivo del estudio: Nuestra hipótesis es que el bloqueo ESP es igual o superior en proporcionar analgesia que el bloqueo QL posterior en cirugía abdominal ambulatoria pediátrica. Diseño. Estudio prospectivo observacional que compara la eficacia analgésica del bloqueo ESP y el bloqueo QLII para cirugía abdominal en pediatría. Pacientes: Se incluyó a un total de 20 pacientes sometidos a cirugía abdominal ambulatoria (urología y cirugía general), ASAI-II, con edad entre 6 meses y 14 años entre marzo y abril de 2018, bajo anestesia general. Todos los participantes fueron asignados al azar para recibir un bloqueo del erector de la columna o del cuadrado lumbar antes del procedimiento. Mediciones: Se midieron el consumo perioperatorio de opioides, el uso de analgesia no opioide y las puntuaciones de dolor. Se documentó parámetros hemodinámicos intraoperatorios (presión arterial y frecuencia cardíaca y oximetría de pulso) así como la presencia de eventos adversos o complicaciones posoperatorias (náuseas o vómitos, depresión respiratoria y sedación). Resultados principales: En ambos grupos, la mayoría de los pacientes refirieron dolor leve o nulo en las primeras 24 h, sin dolor después de las 24 h. Solo 3 pacientes (15%) en el grupo ESP y 2 (10%) en el grupo QLII requirieron analgesia de rescate en el posoperatorio. La estabilidad hemodinámica se mantuvo en ambos grupos. No se informaron complicaciones. Conclusiones: Este estudio respalda la eficacia analgésica y la estabilidad hemodinámica con los bloqueos ESP y QL en el entorno ambulatorio en niños. La superficialidad del punto final de la aguja en ambas técnicas las convierte en una alternativa segura en pediatría.
-
Introduction
Ambulatory surgery has proven to improve health care quality in pediatrics[1]. In general, children are great candidates for procedures performed in this setting for their short duration, less complexity and healthier status of patients. The utilization of regional anesthesia has become a key aspect in ambulatory surgery for its influence in perioperative morbidity and mortality. Appropriate pain management in the postoperative period decreases the use of opiates and its side effects, prevents chronification of pain and its psychological effects such as anxiety, depression and post-traumatic stress syndrome[2]-[4].
Multiple nerve blocks have been described for abdominal surgery and the use of fascial blocks has increased in the past years as part of a multimodal analgesic plan[5], especially in abdominal surgery as part of the enhanced recovery (ERAS) proto- cols[6]-[9]. The quadratus lumborum (QL) block as described in 2007 by Blanco et al[10], consists in the injection of local anesthetics (LA), at the antero-lateral border of the QL muscle. It is believed to allow the spread of LA in between the thoracolumbar fascia, the posterior aspect of the QL muscle and towards the paravertebral space. However spread to the paravertebral space with this block has yet to be proven. In the attempt to obtain a more reliable and higher level blockade, different sites of injection of LA in relation with the QL muscle have been described[11],[12]. New QL block nomenclature refers now to the final injection of LA in relation to the QL (Figure 1) muscle:
anterior (injection of LA anterior to the QL muscle), posterior (injection on the posterior side of the muscle) and lateral (original description in the anterolateral aspect of the muscle). For abdominal surgery, in this institution the posterior QL block is regularly performed, where the injection of local anesthetics is done posteriorly to the QL muscle, closer to the spinal nerves and sympathetic chain providing visceral pain control[13]. More recently, the erector spinae plane block[14] has been described as an analgesic alternative for multiple abdominal procedures in adults and pediatrics. Even though many theories have been described, its mechanism of action remains to be understood, the injection of LA deep to the erector spinae muscle seems to spread anteriorly to the paravertebral space with recent studies demonstrating epidural spread[15]-[17]. This technique appears as a safer alternative when comparing to neuraxial techniques and paravertebral blocks.
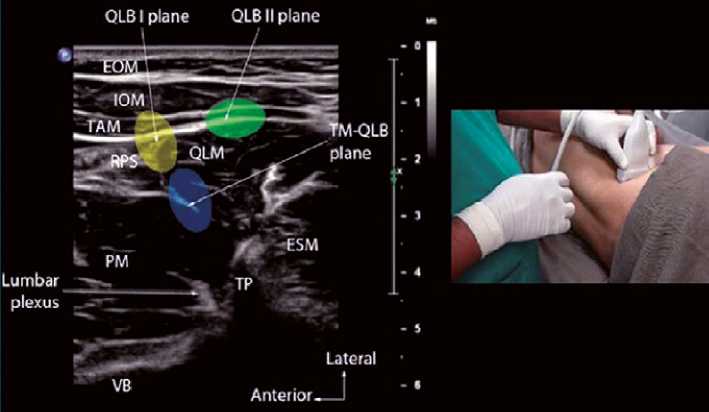
Figure 1. Patient positioning and sonographic image of QL block; EOM: external oblique muscle; IOM: internal oblique muscle; TAM: tranverse abdominis muscle; QLM: quadratus lumborum muscle; RPS: retroperitoneal space; PM: Psoas muscle; TP: transverse process; VB: vertebral body; ESM: erector spinae muscle; TM-QLB: transmuscular quadratus lumborum block.
Erector spinae plane and quadratus lumborum blocks have become part of the daily practice in the pediatric world, how- ever comparison studies in the pediatric population are scarce. We present a prospective observational study comparing the analgesic efficacy of ESP block and QLII block for abdominal surgery in pediatrics. Our hypothesis is that ESP block is equal or superior in providing analgesia than the posterior QL block in abdominal surgery in ambulatory surgery. Our primary out- come is to evaluate analgesic efficacy between each group by analyzing pain scores, opiate consumption, need for analgesic rescue in the first 24. As secondary outcomes we evaluated hemodynamic changes intraoperatively, incidence of adverse effects intraoperatively and postoperatively, and presence of postoperative sedation with each technique.
-
Methods
Ethics committee approval from Hospital de Niños Dr. Orlando Alassia was obtained to perform the study. Patients undergoing ambulatory abdominal surgery (urology and general surgery), ASAI-II, age between 6 months and 14 years old with- in March-April 2018, under general anesthesia were included. Informed consent was obtained from all parents. All partici- pants were randomized in a 1:1 fashion to 2 groups: Group A (ESP block) and Group B (QL2 block). Each group had 10 patients in total. Exclusion criteria were allergies to LA, coagu- lopathy, infection on site of puncture, ASA III-IV and refusal to have regional anesthesia or to participate in the study. Pain was evaluated utilizing numeric rating scale score for patient > 6 years-old, LLANTO scale was used for patients < 6 years-old. Pain scores at 10, 30 mins, 4, 12 and 24 h post-surgery were documented and defined as mild/tolerable (0-3), moderate (> 3-6), severe (7-10). Tramadol 0.5 mg/kg and morphine 0.1 mg/ kg were available as rescue if needed for pain control and its use was recorded.
Intraoperative hemodynamics (blood pressure and heart rate) and pulse oximeter were recorded for both groups, before and immediately after placement of nerve block. For adverse events we evaluated incidence of nausea or vomiting, respiratory depression (defined as a respiratory rate lower than the inferior limit per age and O2 saturation less than 92%) and presence of apnea (defined by absence of breathing > 20 secs). Sedation was evaluated by Ramsay scale defining appropriate sedation with a Ramsay score from 2-4 (1. anxious/agitated; 2. cooperative, calm and oriented; 3. responds to verbal stimuli; 4. sleeping, arousable to sounds or light; 5. slow response to sounds or light; 6. no response).
No medication, analgesics or sedatives, were given preoperatively. Intraoperatively, standard monitoring, as well as inhaled induction with sevofluorane was utilized for all patients. Once intravenous access was obtained, patients received propofol 2 mg/kg, fentanyl 1 mcg/kg, mivacurium 0.2 mg/kg and dexamethasone 0.2 mg/kg followed by either endotracheal intubation or supraglotic device placement for airway management. For maintenance of anesthesia sevofluorane 1 CAM and remifentanyl 0.5 mcg/kg/min were utilized and titrated to anesthetic
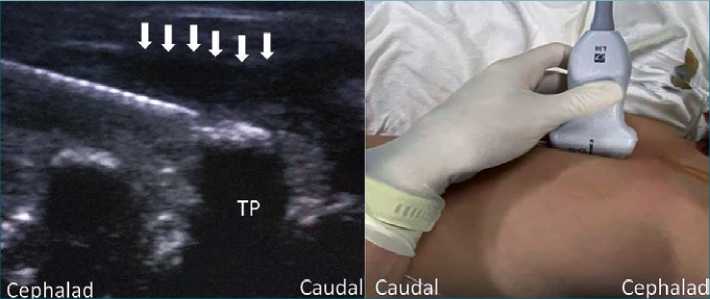
Figure 2. Patient positioning and sonographic image of ESP block; TP: transverse process. Ar- rows: pointing local anesthetic injection.
-
Results
Twenty patients were included and distributed equally in 2 requirements and hemodynamic parameters. Patients received dipirone 20 mg/kg and diclofenac 1 mg/kg or ketorolac 1mg/ kg for analgesia. Acetaminophen (7.5 mg/kg in < 10 kg or 15 mg/kg in > 10 kg) in addition to dipirone was given in patients with allergy to non-steroidal anti-inflammatory drugs (NSAIDs).
All nerve blocks were placed after induction of general anesthesia with sterile technique. A high frequency US (6-15 MHz, sonosite Edge II) was used. Surgical incision was performed 15mins after block placement in all cases, and patients were extubated or supraglotic device removed once patient was awake and responsive.
Posterior QL block technique (Figure 1): Patient was placed either supine with a roll underneath the hip of the side to be blocked or on a lateral side, with the side to block upwards. A high frequency US probe was placed transverse oriented at the level of the posterior axillary line, between the rib border and the iliac crest. Once the abdominal wall muscles and QL muscle were identified an echogenic needle was inserted in plane from anterior to posterior until reaching the posterior aspect of the quadratus lumborum muscle. Saline 1ml was administered to confirm tip placement, followed by injection of 0.5ml/Kg of a 1:1 mix of bupivacaine 0.25%: lidocaine 1% in aliquots. Spread of LA was visualized with US.
ESP block technique (Figure 2):
Patients were placed on the lateral side, with side to block upwards. The US probe was place at the level of T6-T7, parallel to the spine over the transverse processes. Once the tip of the transverse process was identified, an echogenic needle was inserted until contacting the bony structure, in plane from cephalad to caudad deep to the erector spine muscle. Saline 1 ml was used to confirm and dissect the plane followed by injection of 0.5 ml/kg of a 1:1 mix of bupivacaine 0.25%: lidocaine 1% in aliquots. Spread of LA cephalad and caudad was identified with US.
Statistical analysis: Info-stat was used for statistical analysis. Median and SD were reported for continue variables and percentage for categorical variables. Wilconson test was used for comparison of median for independent variables and chisquare test for comparison of percentages between groups. Confident value of a = 0.05 was used.
groups: ESP and posterior QL block. Male distribution in each group was 80% and 70% respectively. Median age was 4 years old (SD ± 4 ys) for ESP group and 4.1 years old (SD ± 4.4 ys) for QL group. No statistical significant difference was found between groups (p = 0.531). Type of surgeries is presented in Table 1.
All patients in ESP group were ASA I, whereas 80% were ASA1 and 20% ASA2 in the QL group. Postoperative pain scores are presented in Table 2.
In both groups the majority of patients reported mild or no pain in the first 24 h with no pain after 24 h; with any statistical differences between groups. Only 3 patients (15%) in the ESP group and 2 (10%) in the QLII group required rescue analgesia postoperatively (tramadol 0.5 mg/kg), mean time after end of surgery 48.3 min.
As secondary outcomes we evaluated hemodynamic variables presented in Table 3.
The degree of sedation at 10, 30 min and 4 h was statistically similar in both groups. In the first 10mins a grade 3 and 4 was predominant in both groups; at 30 min grade 3 was predominant whereas at 4 h grade 2 was the predominant score. No complications were reported, but interestingly bilateral analgesia was reported by one of the patients in the ESP group, and deep sedation with a Ramsay score of 3 for 2 h after the procedure was evidenced in a patient in the QL block group.
Table 1. Type of surgeries
| Type of surgery | Number | Percentage |
| Appendectomy | 1 | 5 |
| Orchiopexy | 4 | 20 |
| Correction of phimosis | 1 | 5 |
| Inguinal hernia repair | 9 | 45 |
| Hydrocele repair | 2 | 10 |
| Hypospadia repair | 1 | 5 |
| Oophorectomy | 1 | 5 |
| Ureteral reimplant | 1 | 5 |
-
Discussion
This study concurs with current evidence of good pain control with ESP and QL block for abdominal surgery[7]. Moreover, it provides evidence of the successful application of these blocks in the ambulatory setting, with minimal sedation and no complications such as nausea and vomiting that could delay discharge time. In addition, this study adds to the literature in pediatrics, where the ESP block has been adapted widely, but the lack of comparison studies continues to be in need. Recently Aksu et al[7], compared the analgesic efficacy of these blocks for lower abdominal surgery concluding that both blocks provide adequate analgesia; however in our study we compare not only the analgesic efficacy, but also the hemodynamic changes and evidence of sedation in the postoperative period with both blocks. When analyzing our results, only 3 patients on the ESP block and 2 patients in the QL block group required rescue analgesia with tramadol in the immediate postoperative period (mean ~43 min) supporting the equivalent analgesic efficacy of these blocks. Pain control was excellent with both blocks, evidenced by the presence of no pain or mild pain in most patients in the first 24 h and no pain reported afterwards.
Table 2. Pain scores presented in percentage
| Time | PS | ESP (n = 10) | QL (n = 10) | p-value |
| 10 min | No pain | 90% | 90% | 0.368 |
| Mild | 10% | 0% | ||
| Moderate | 0% | 10% | ||
| Severe | 0% | 0% | ||
| 30 min | No pain | 90% | 80% | 0.383 |
| Mild | 0% | 10% | ||
| Moderate | 10% | 10% | ||
| Severe | 0% | 0% | ||
| 4 h | No pain | 100% | 90% | 0.305 |
| Mild | 0% | 0% | ||
| Moderate | 0% | 10% | ||
| Severe | 0% | 0% | ||
| 12 h | No pain | 90% | 100% | 0.305 |
| Mild | 10% | 0% | ||
| Moderate | 0% | 0% | ||
| Severe | 0% | 0% | ||
| 24 h | No pain | 100% | 100 | |
| Mild | 0% | 0% | ||
| Moderate | 0% | 0% | ||
| Severe | 0% | 0% |
Table 3. Hemodynamic measurements
| Variables | Time | ESP (n=10) | QLB II (n=10) | p-value |
| SBP (mmHg) | Pre block | 81.0 ± 11.7 | 90.5 ± 14.2 | 0.189 |
| Post block | 72.8 ± 11.4 | 81.3 ± 9.2 | 0.167 | |
| DBP (mmHg) | Pre block | 50.8 ± 5.8 | 53.5 ± 11.6 | 0.662 |
| Post block | 44.2 ± 6.5 | 45.0 ± 8.5 | 0.999 | |
| MAP (mmHg) | Pre block | 59.1 ± 4.6 | 60.5 ± 5.5 | 0.661 |
| Post block | 53.6 ± 6.6 | 56.1 ± 3.9 | 0.560 | |
| Heart rate | Pre block | 99.1 ± 16.7 | 111.1 ± 12.1 | 0.104 |
| Post block | 84.9 ± 17.5 | 98.8 ± 13.3 | 0.110 | |
| SatO2 | Pre block | 1.00 ± 0.01 | 0.99 ± 0.01 | 0.150 |
| Post block | 1.00 ± 0.01 | 0.99 ± 0.01 | 0.226 |
Systolic Blood Pressure (SBP); Diastolic Blood Pressure (DBP); Median Blood pressure (MAP); Oxygen Saturation (SatO2) (mean ± SD).
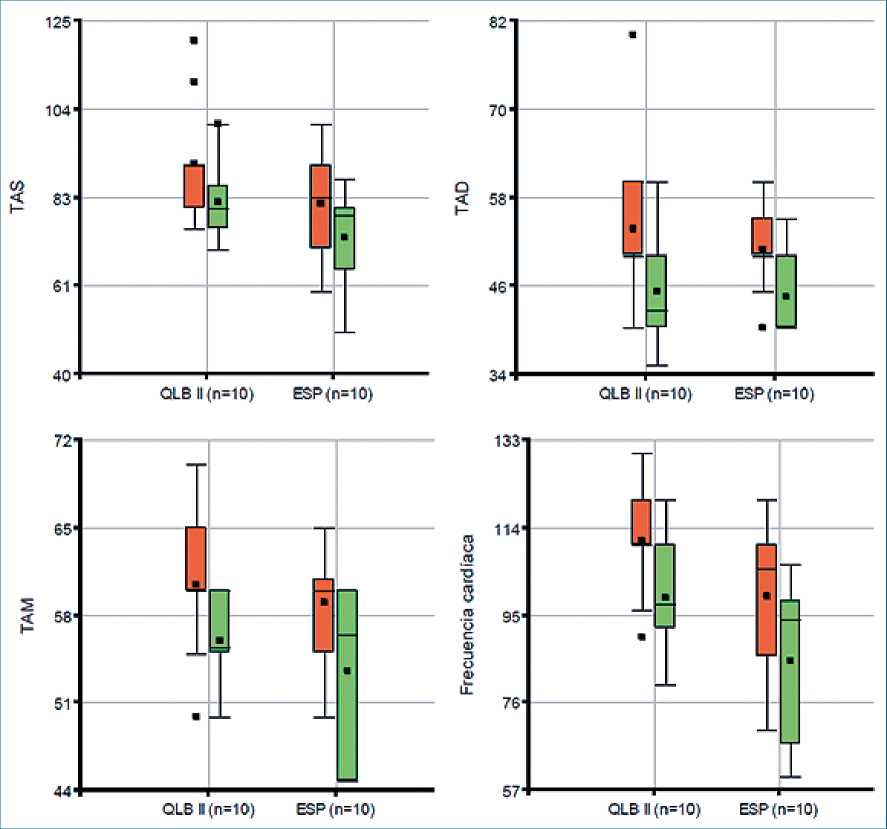
Figure 3. Hemodynamic measurements. TAS: Systolic blood pressure; TAD: Diastolic blood pressure; TAM: Median blood pressure; Frecuencia cardiaca: cardiac frequency (heart rate).
QLII blocks for its superficial approach and effectiveness in providing somatic and visceral pain control for abdominal surgery, have been an attractive and widely used technique in the pediatric population. Likewise, the ESP block due to its simplicity and favorable safety profile, away from important structures, is becoming the “go to” block in the pediatric population. These 2 blocks have the characteristic that either mechanism of action is not understood completely, with many cadaveric studies showing contradictory results, whether they have paravertebral spread or not[18],[19], and some studies going forward in demonstrating epidural spread with ESP block [15],[16],[20]. In spite of that, this valuable information is hard to extrapolate to living subjects were the characteristics of muscles and fascias may play an important role in the clinical effect evidenced with this technique, especially in the pediatric population. Other mechanisms for ESP block cited are spread of LA anteriorly to the paravertebral space blocking the anterior and posterior rami of the spinal nerves (somatic pain control) and the sympathetic chain (visceral pain control). One of our patients in the ESP group reported bilateral analgesia, sighting a possible epidural spread with this block; however, this is only one case, and the limited sample cannot affirm that indeed the patient had epidural spread. However, this is something worth investigating. All these arguments continue to highlight the need for further research in this area.
As a secondary outcome we evaluated the hemodynamic changes that may be caused when using these blocks (Table 3). Blood pressure (BP) levels were higher for the QL groups, but it was not statistically significant. The box plot graphs (Figure 3) indicate that the values were higher prior to receiving the block than afterward, and that the QL block group had higher values throughout. These results may aid the anesthesiologist decision when selecting an analgesic technique, especially in sicker patients, where hemodynamic stability is key.
The clinical experience in this institution has been that patient receiving ESP block have had sedation in the postoperative period, leading the authors into investigating possible effect of epidural spread as well as lidocaine absorption in those patients as described in current literature[15],[16]. The use of epidural lidocaine has been associated with sedation and less requirements of anesthetics for its systemic absorption from the epidural space and deafferentation from neuraxial blockade. However more studies are needed to corroborate this hypothesis. The lack of hemodynamic changes with both blocks can also challenge this hypothesis, at least in the oldest patients where sympathetic blockade could manifest with hypotension and bradycardia if epidural spread is suspected. None of these elements were evidenced in our study. Until this is not elucidated, we do not recommend this block as a substitute to neuraxial technique. In addition, we reported a deep sedation status (Ramsay score of 3) in a patient in the QL group, sup- porting a major implication of systemic absorption in explaining this symptom, since the QL block plane is highly vascularized and reports of complications such as hematomas have been described[21].
Despite being a prospective study, the main limitation of our study is the small sample evaluated. However, this is the first report to evaluate these blocks in ambulatory surgery and its hemodynamic repercussion. More studies are needed to investigate the efficacy and safety of these blocks in children. Our results could be used in rigorous sample size calculation in planning a subsequent, more extensive prospective study.
-
Conclusion
This study supports the analgesic efficacy and hemodynamic stability obtained with both techniques for abdominal surgery in the ambulatory setting in children. The superficiality of the needle end point in both techniques makes them a safe alternative in pediatrics. We realize that the small sample utilized in this study may limit the generalization or conclusions, but this could serve as a start point for future studies.
Declarations of interest: none.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
1. Stein AL, Baumgard D, Del Rio I, Tutiven JL. Updates in Pediatric Regional Anesthesia and Its Role in the Treatment of Acute Pain in the Ambulatory Setting. Curr Pain Headache Rep. 2017 Feb;21(2):11. https://doi.org/10.1007/s11916-017-0614-z PMID:28251525
2. Kessler J, Marhofer P, Hopkins PM, Hollmann MW. Peripheral regional anaesthesia and outcome: lessons learned from the last 10 years. Br J Anaesth. 2015 May;114(5):728–45. https://doi.org/10.1093/bja/aeu559 PMID:25690833
3. Polaner DM, Taenzer AH, Walker BJ, Bosenberg A, Krane EJ, Suresh S, et al. Pediatric Regional Anesthesia Network (PRAN): a multi-institutional study of the use and incidence of complications of pediatric regional anesthesia. Anesth Analg. 2012 Dec;115(6):1353–64. https://doi.org/10.1213/ANE.0b013e31825d9f4b PMID:22696610
4. Marhofer P, Harrop-Griffiths W, Willschke H, Kirchmair L. Fifteen years of ultrasound guidance in regional anaesthesia: Part 2-recent developments in block techniques. Br J Anaesth. 2010 Jun;104(6):673–83. https://doi.org/10.1093/bja/aeq086 PMID:20418267
5. Dontukurthy S, Mofidi R. The Role of Interfascial Plane Blocks in Paediatric Regional Anaesthesia: A Narrative Review of Current Perspectives and Updates 2020. https://doi.org/10.1155/2020/8892537..
6. Yeap YL, Wolfe JW, Kroepfl E, Fridell J, Powelson JA. Transversus abdominis plane (TAP) block for laparoscopic live donor nephrectomy: continuous catheter infusion provides no additional analgesic benefit over single-injection ropivacaine. Clin Transplant. 2020 Jun;34(6):e13861. https://doi.org/10.1111/ctr.13861 PMID:32198963
7. Aksu C, Şen MC, Akay MA, Baydemir C, Gürkan Y. Erector Spinae Plane Block vs Quadratus Lumborum Block for pediatric lower abdominal surgery: A double blinded, prospective, and randomized trial. J Clin Anesth. 2019 Nov;57:24–8. https://doi.org/10.1016/j.jclinane.2019.03.006 PMID:30851499
8. Chin KJ, Malhas L, Perlas A. The Erector Spinae Plane Block Provides Visceral Abdominal Analgesia in Bariatric Surgery: A Report of 3 Cases. Reg Anesth Pain Med. 2017 May/Jun;42(3):372–6. https://doi.org/10.1097/AAP.0000000000000581 PMID:28272292
9. Wang Y, Wang X, Zhang K. Effects of transversus abdominis plane block versus quadratus lumborum block on postoperative analgesia: a meta-analysis of randomized controlled trials. BMC Anesthesiol. 2020 May;20(1):103. https://doi.org/10.1186/s12871-020-01000-2 PMID:32366275
10. Blanco R. 271: Tap block under ultrasound guidance: the description of a “no pops” technique. Reg Anesth Pain Med. 2007;32(5):130–130. https://doi.org/10.1016/j.rapm.2007.06.268.
11. Ueshima H, Otake H, Lin JA. Ultrasound-Guided Quadratus Lumborum Block: An Updated Review of Anatomy and Techniques. BioMed Res Int. 2017;2017:2752876. https://doi.org/10.1155/2017/2752876 PMID:28154824
12. Elsharkawy H, El-Boghdadly K, Barrington M. Quadratus Lumborum Block: Anatomical Concepts, Mechanisms, and Techniques. Anesthesiology. 2019 Feb;130(2):322–35. https://doi.org/10.1097/ALN.0000000000002524 PMID:30688787
13. Öksüz G, Bilal B, Gürkan Y, Urfalioğlu A, Arslan M, Gişi G, et al. Quadratus Lumborum Block Versus Transversus Abdominis Plane Block in Children Undergoing Low Abdominal Surgery: A Randomized Controlled Trial. Reg Anesth Pain Med. 2017 Sep/Oct;42(5):674–9. https://doi.org/10.1097/AAP.0000000000000645 PMID:28759502
14. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The Erector Spinae Plane Block: A Novel Analgesic Technique in Thoracic Neuropathic Pain. Reg Anesth Pain Med. 2016 Sep-Oct;41(5):621–7. https://doi.org/10.1097/AAP.0000000000000451 PMID:27501016
15. Schwartzmann A, Peng P, Antunez Maciel M, Forero M. Bilateral erector spinae plane block (ESPB) epidural spread. Reg Anesth Pain Med. 2019 Jan;44(1):131. https://doi.org/10.1136/rapm-2018-000030 PMID:30640666
16. Lapalma J, Palazzi L, Forero M, Schwartzmann A. Sitio de acción del bloqueo del plano del músculo erector de la columna (ESP) – Estudio mediante resonancia magnética en un niño. Rev Esp Anestesiol Reanim. 2020;•••: https://doi.org/10.1016/j.redar.2020.06.017.
17. Chin KJ, Adhikary S, Sarwani N, Forero M. The analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017 Apr;72(4):452–60. https://doi.org/10.1111/anae.13814 PMID:28188621
18. Yang HM, Park SJ, Yoon KB, Park K, Kim SH. Cadaveric Evaluation of Different Approaches for Quadratus Lumborum Blocks. Pain Res Manag. 2018 Jun;2018:2368930. https://doi.org/10.1155/2018/2368930 PMID:29991972
19. Adhikary SD, Bernard S, Lopez H, Chin KJ. Erector Spinae Plane Block Versus Retrolaminar Block: A Magnetic Resonance Imaging and Anatomical Study. Reg Anesth Pain Med. 2018 Oct;43(7):756–62. https://doi.org/10.1097/AAP.0000000000000798 PMID:29794943
20. Saadawi M, Layera S, Aliste J, Bravo D, Leurcharusmee P, Tran Q. Erector spinae plane block: A narrative review with systematic analysis of the evidence pertaining to clinical indications and alternative truncal blocks. J Clin Anesth. 2021 Feb;68:110063. https://doi.org/10.1016/j.jclinane.2020.110063 PMID:33032124
21. Visoiu M, Pan S. Quadratus lumborum blocks: two cases of associated hematoma. Paediatr Anaesth. 2019 Mar;29(3):286–8. https://doi.org/10.1111/pan.13588 PMID:30664311

 ORCID
ORCID