María Fernanda Avendaño Navarro MD. 1 , Andrés Rocha Romero MD. 1 ,*, Ricardo Aguilar Ureña MD. 1 , Mario Fajardo Pérez MD. 2 , Rodrigo Benavides Cordero MD. 1 , Karla Espinoza Morales MD. 1
Recibido: 11-01-2021
Aceptado: 15-04-2021
©2022 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 51 Núm. 1 pp. 67-74|https://doi.org/10.25237/revchilanestv5128121711
PDF|ePub|RIS
Serie de casos: Efecto de triamicinolona en anestesia regional fast track para reemplazo de rodilla
Abstract
Background: Many adjuvants have been studied to improve the quality of analgesia and to prolong its duration. To date, there are no reports on the use of triamcinolone. Case: We present a brief report of 10 patients receiving a single shot ACB and IPACK blockade with a small dose of triamcinolone for Fast-Track Knee Replacement to prolong analgesia. Conclusión: We think this is a valuable opioid-sparing option, cheaper than new adjuvants, and safer than the use of continuous infusion. This technique should be evaluated in clinical trials.
Resumen
Antecedentes: Muchos agentes farmacológicos que se utilizan como adyuvantes en la anestesia regional han sido estudiados con el fin de mejorar la calidad de la analgesia y prolongar la duración del efecto. Hoy en día no existen reportes del uso de triamcinolona en dichos procedimientos. Caso: Consiste en el reporte breve de 10 pacientes que se les realizo ACB además de un bloqueo IPACK con una sola inyección de anestesia local con el adyuvante triamcinolona, con el objetivo de prolongar la analgesia en la cirugía de reemplazo de rodilla Fast-Track. Conclusión: Consideramos que una valiosa opción para el ahorro de opioide, más económica que las nuevas opciones de mercado y más seguras que el uso de infusiones continuas. Esta técnica debería ser evaluada en ensayos clínicos.
Pain after orthopedic surgery remains a significant challenge for the anesthesiologist. Higher preoperative pain scores, depression, and younger age are independent predictors of severe postoperative pain. In response to knee joint arthroplasty pain, the multimodal approach is claimed to be the most appropriate option, and this includes peripheral nerve blocks[1]. One limitation of regional anesthesia for these procedures is the finite duration of single-injection techniques. One more concern about this kind of surgery is the rehabilitation process. Novel blocks like infiltration between the popli- teal artery and capsule of the knee (IPACK) and adductor canal block (ACB) are recommended as a motor sparing strategy. We present a report of 10 patients receiving a single shot adductor canal and infiltration between the popliteal artery and capsule of the knee blockade with triamcinolone for Fast-Track Knee Replacement. Written informed consent was obtained from the participants for this report.

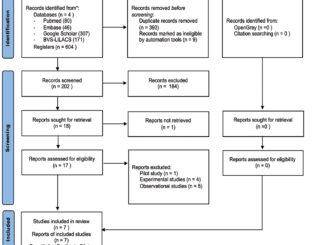
Figure 1: A. Ultrasound image of adductor canal block. S; Sartorius; AL, Adductor longus; VM, Vastus medialis; FV, Femoral vessels; B. Ultrasound image of infiltration between the popliteal artery and capsule of the knee. S, Sartorius; AL, Adductor longus; VM, Vastus medialis; FV, Femoral vessels; SN, Sciatic nerve; GNM, Gastrocnemius muscle; PV, Popliteal vein; PA, Popliteal artery; FV, Femoral condyle.
Patients admitted for fast-track knee replacement were offered spinal plus regional anesthesia as a component of a multimodal analgesic regimen. Spinal anesthesia was performed with 8 mg of levobupivacaine. Intravenous sedation with midazolam (0,06 mg/kg) was administered to all patients under standard noninvasive monitorization. In 10 cases, a single-injection IPACK and ACB was performed using 20 mL of 0.25%
bupivacaine with 20 mg of triamcinolone acetonide for each one in all cases. No surgical infiltration was done and revision surgeries were not included for this study. Nonsteroidal anti- inflammatory drugs were given to all patients as part of multi- modal management.
IPACK blocks were performed under ultrasound guidance with a curvilinear low-frequency probe (GE LOGIQTM e Portable Ultrasound Machine) using a 22 G x 80 mm echogenic needle (SonoPlexTM STIM, PAJUNK) and the patient in supine position with external rotation of the leg. The popliteal artery was identified in a short-axis view, at the popliteal crease, and moved cephalad at the level where the condyles merge with the shaft of the femur. After identifying the space between the femur and popliteal artery, the needle was advanced in plane from medial to lateral. The tip was positioned at the middle of the femur and near the lateral border near the periosteum. After negative aspiration, the local anesthetic mixture was injected in 2-mL increments while observing for an adequate fluid spread. Avoiding extensive injectate spread to the components of the sciatic nerve.
For the ACB, the patient was in the supine position. A linear high-frequency ultrasound probe was placed over the midthigh to visualize the sartorius muscle, the vastus medialis muscle and adductor longus muscle in short-axis. At this level, the needle was inserted in-plane from lateral to medial. After negative aspiration, the same solution was injected in 2-mL increments while observing for an adequate fluid spread. All blocks were performed by residents, supervised by experienced specialists (Figure 1).
The demographic information, ASA physical status classification, body mass index (BMI), and surgery side were noted. The numeric rating scale (NRS) for rest and dynamic pain, 4-point Likert patient satisfaction score (1, dissatisfied; 2, slightly dissatisfied; 3, slightly satisfied; 4, satisfied), the cumulated rescue opioid doses in postoperative management (described oral morphine equivalent OME), and the time to first opioid dose were collected. The follow-up time was 72 h. One-week later patients were contacted to inquire about complications.
The present case series suggest that the addition of triamcinolone to levobupivacaine resulted in long-lasting analgesia of both ACB and IPACK block. Ten patients were included, three men and seven women. The mean age was 77.9 years, and the mean BMI was 28.7 kg/m (Table 1).
The median Numeric Rating Scale (NRS) for rest pain was 0 at 24, 48, and 72 hours. The median NRS for dynamic pain was 2 in the same time frame, respectively. Only two patients required breakthrough opioids due to inadequate control of dynamic pain, at 12 and 60 hours, for a total oral morphine equivalent (OME) of 200 and 100, respectively. Based on a 4-point Likert scale (1, dissatisfied; 2, slightly dissatisfied; 3, slightly satisfied; 4, satisfied), this approach resulted in adequate patient satisfaction (Table 2). Block failure was reported in one case, requiring a second block 12 h later. One week later, patients were contacted to inquire about complications. None was reported.
The finite duration of single-injection techniques is a limitation of regional anesthesia in acute postoperative pain management. There are three main methods to prolong the duration of regional anesthetic techniques[2]. The first is to include local anesthetic adjuncts, but the expected prolongation usually is no more than eight hours[3]. The second is continuous catheter techniques, but it is more complex to perform and requires an organized follow-up to decrease infection and migration risk.
| Table 1. Characteristics of patients | |||||
| Cases | ASA | BMI | Sex | Age | Side |
| 1 | II | 28.2 | F | 82 | R |
| 2 | II | 27.5 | M | 81 | L |
| 3 | II | 29.6 | M | 75 | L |
| 4 | I | 34.5 | F | 73 | R |
| 5 | II | 27.6 | F | 88 | R |
| 6 | I | 28.4 | F | 73 | R |
| 7 | II | 26.7 | F | 77 | R |
| 8 | II | 29.6 | F | 82 | R |
| 9 | II | 28.3 | F | 73 | L |
| 10 | II | 26.7 | M | 75 | L |
Abbreviations: R, right; L, left; M, male; F, female.
| Table 2. Summary of patient outcomes | |||||||||
| Numeric Rating Scale (Rest / Dynamic) | OME 72 h | Time to first opioid dose (h) | Likert scale | ||||||
| Recovery | 12 h | 24 h | 36 h | 48 h | 60 h | 72 h | |||
| 0/0 | 1/1 | 0/0 | 0/0 | 0/0 | 0/0 | 0/2 | 0 | NR | 4 |
| 0/0 | 0/0 | 0/0 | 0/0 | 0/0 | 0/0 | 1/2 | 0 | NR | 4 |
| 0/0 | 2/3 | 2/3 | 0/0 | 0/2 | 0/2 | 0/2 | 0 | NR | 4 |
| 0/0 | 0/0 | 0/2 | 0/0 | 0/3 | 1/4 | 0/2 | 100 | 60 | 4 |
| 0/0* | 0/0 | 0/3 | 0/0 | 2/4 | 0/3 | 3/6 | 0 | NR | 3 |
| 0/0 | 0/0 | 0/2 | 0/0 | 0/2 | 0/2 | 0/1 | 0 | NR | 3 |
| 0/0 | 0/0 | 0/0 | 0/0 | 0/0 | 0/2 | 0/2 | 0 | NR | 4 |
| 0/3 | 0/3 | 0/3 | 0/2 | 0/2 | 0/2 | 0/2 | 0 | NR | 4 |
| 0/0 | 0/0 | 0/0 | 0/0 | 0/0 | 0/2 | 0/2 | 0 | NR | 4 |
| 0/0 | 2/8 | 2/8** | 0/4 | 0/2 | 0/8 | 0/8 | 200 | 12 | 2 |
Abbreviations: BMI, body mass index; **second ACB performed; NR, not required.
*patient with sequelae of poliomyelitis; OME, oral morphine equivalent.
The last is using sustained-release local anesthetic.; like liposomal bupivacaine. This product is approved for interscalene brachial plexus block, transversus abdominis plane block, and surgical infiltration, but it is expensive.
Regional anesthesia techniques are evolving to facilitate early ambulation after this kind of surgeries[4]. Although the physical and chemical compatibility of triamcinolone with common local anesthetics has been described[5], it is usually reserved just for chronic pain management procedures like chronic musculoskeletal injections[6]. Triamcinolone is a corticosteroid of high molecular weight and complex structure used for prolonging analgesia of local anesthetics, but little is known about its effectiveness in acute postoperative pain management. The perineural administration of triamcinolone is known to reduce the spontaneous ectopic discharges that arise in experimental nerve end neuromas and prevents the further development of ectopic impulses in freshly severed nerves[7].
When using adjuvants, caution is recommended, as only epinephrine is Food and Drug Administration (FDA) approved for perineural use. Neurotoxic effect of steroids is controversial; some basic science studies describe peripheral nerve damage, most of the time related to preservatives (triamcinolone contains benzyl alcohol), while other studies suggest neuroprotective effects[8].
We found no studies describing the addition of triamcinolone for lower extremity regional anesthetic techniques. Previous reports for scalp, greater occipital nerve block, ilioinguinal and interscalene brachial plexus blocks remain controversial[9]-[11]. A clinical prospective study by Webb[11] found statistically longer pain relief and no difference between triamcinolone and a control group in terms of complications for interscalene brachial plexus block. As mentioned above, most patients benefit long-lasting pain relief of 72 h, and we did not find any complications. Furthermore, rescue opioid dose was required in just two patients at 60 h and 48 h.
We think that the use of perineural triamcinolone as local anesthetic adjunct for improving postoperative pain experience in fast-track knee replacement is a valuable opioid-sparing option. It is cheaper than liposomal bupivacaine and easier to perform than continuous catheter techniques.
The presented cases illustrate the efficacy and usefulness of adding a small dose of triamcinolone in ACB and IPACK block for the management of postoperative pain in fast-track knee replacement surgery. Further larger scaled studies are needed to clarify the optimal dose, safety profile and to compare the efficacy of this technique with other modalities such as continuous infusions or liposomal bupivacaine.
Author’s financial disclosure: The authors declare they do not have any conflicts of interest relevant to this present manuscript.
Conflict of Interests: No conflicts of interests are declared.
Funding/Support: This study did not receive any funds or financial support.
Patient Consent: A consent form was obtained from the patient for publication of this report.
1. O’Donnell R, Dolan J. Anaesthesia and analgesia for knee joint arthroplasty. BJA Educ. 2018 Jan;18(1):8–15. https://doi.org/10.1016/j.bjae.2017.11.003 PMID:33456789
2. Albrecht E, Chin KJ. Advances in regional anaesthesia and acute pain management: a narrative review. Anaesthesia. 2020 Jan;75(S1 Suppl 1):e101–10. https://doi.org/10.1111/anae.14868 PMID:31903582
3. Desai N, Kirkham KR, Albrecht E. Local anaesthetic adjuncts for peripheral regional anaesthesia: a narrative review. Anaesthesia. 2021 Jan;76(S1 Suppl 1):100–9. https://doi.org/10.1111/anae.15245 PMID:33426668
4. Jackson JD, Cotton L, Turkington M, Leblanc D, Kelley S. Physical and Chemical Compatibility of Extended-Release Triamcinolone Acetonide (TA-ER) with Common Local Anesthetics. Adv Ther. 2019 Mar;36(3):652–61. https://doi.org/10.1007/s12325-019-0878-2 PMID:30706409
5. Xu L, Leng JC, Elsharkawy H, Hunter OO, Harrison TK, Vokach-Brodsky L, Kumar G, Funck N, Hill JN, Giori NJ, Indelli PF, Kou A, Mariano ER. Replacement of Fascia Iliaca Catheters with Continuous Erector Spinae Plane Blocks Within a Clinical Pathway Facilitates Early Ambulation After Total Hip Arthroplasty. Pain Med. 2020,1;21(10):2423-2429. https://doi.org/10.1093/pm/pnaa243.
6. Shah A, Mak D, Davies AM, James SL, Botchu R. Musculoskeletal Corticosteroid Administration: current Concepts. Can Assoc Radiol J. 2019 Feb;70(1):29–36. https://doi.org/10.1016/j.carj.2018.11.002 PMID:30691559
7. Van Boxem K, Rijsdijk M, Hans G, de Jong J, Kallewaard JW, Vissers K, et al. Safe Use of Epidural Corticosteroid Injections: Recommendations of the WIP Benelux Work Group. Pain Pract. 2019 Jan;19(1):61–92. https://doi.org/10.1111/papr.12709 PMID:29756333
8. Kukreja P, MacBeth L, Feinstein J. Local Anesthetic Additives for Regional Anesthesia: a Review of Current Literature and Clinical Application. Curr Anesthesiol Rep. 2019;9(3):314–20. https://doi.org/10.1007/s40140-019-00334-z.
9. Kim HS, Lee SJ, Kim CS, Kim JT. Effect of triamcinolone added to scalp nerve block for postoperative pain management of Moyamoya disease. Korean J Anesthesiol. 2011 Aug;61(2):173–4. https://doi.org/10.4097/kjae.2011.61.2.173 PMID:21927693
10. Ashkenazi A, Matro R, Shaw JW, Abbas MA, Silberstein SD. Greater occipital nerve block using local anaesthetics alone or with triamcinolone for transformed migraine: a randomised comparative study. J Neurol Neurosurg Psychiatry. 2008 Apr;79(4):415–7. https://doi.org/10.1136/jnnp.2007.124420 PMID:17682008
11. Webb BG, Sallay PI, McMurray SD, Misamore GW. Comparison of Interscalene Brachial Plexus Block Performed With and Without Steroids. Orthopedics. 2016 Nov;39(6):e1100–3. https://doi.org/10.3928/01477447-20160819-02 PMID:27575034

 ORCID
ORCID