Carolina Cardoso1,* Joao M. Rego1, Cristiana G. Pereira1, Hélder P. Cardoso1, Fernando P. Moura1
Recibido: 08-12-2019
Aceptado: 19-12-2019
©2023 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 52 Núm. 2 pp. 251-254|https://doi.org/10.25237/revchilanestv5206021048
PDF|ePub|RIS
Videolaringoscopia vigil puede ser una alternativa
a fibrobroncoscopía vigil?
Abstract
Awake fiberoptic intubation has for many years been the gold-standard in patients with difficult airway. Videolaryngoscopy has already shown some advantages in patients with a difficult airway and compared to fiberoptic intubation it uses a technically simpler equipment and it is easier and quicker to learn. The aim of this article is to discuss awake videolaryngoscopy as an alternative to awake fibreoptic intubation and some practical aspects regarding regional anesthesia. We report the successful tracheal intubation of 10 awake patients using the videolaryngoscope C-MAC® D-blade. Administration of atropine and sedation with alfentanil and midazolam was performed. Anesthesia was achieved with spray applied on the surface of the tongue and oropharynges, a bilateral submucous block of the glossopharyngeal nerve and a transtracheal injection. The technique was successful on the first attempt in the 10 cases. Regional anaesthesia and sedation were sufficient, once ventilatory and hemodynamic stability were observed, except in 1 case where tachycardia, hypertension and mild agitation were noted, without however compromising the procedure and with no need for further intervention. Our cases series suggest the hypothesis that videolaryngoscopy can be an alternative to fiberoptic intubation in awake patients. We also suggest it is easier to learn and can be performed with a similar success, security and comfort of patients.
Resumen
La intubación con fibroscopia con el paciente vigil ha sido, durante muchos años, el estándar en pacientes con vías aéreas difíciles. La videolaringoscopia ya ha mostrado algunas ventajas en pacientes con vía aérea difícil y, en comparación con la fibroscopia, utiliza un equipo técnicamente más simple y es más fácil y rápido de aprender. El objetivo de este artículo es discutir la videolaringoscopia con el paciente vigil como una alternativa a la fibroscopia y algunos aspectos prácticos relacionados con la anestesia regional. Reportamos la intubación traqueal exitosa de 10 pacientes vigil usando el videolaringoscopio C-MAC® D-bladeTM. Se realizó la administración de atropina y sedación con alfentanilo y midazolam. La anestesia se logró con un aerosol aplicado sobre la superficie de la lengua y orofaringe, un bloqueo submucoso bilateral del nervio glosofaríngeo y una inyección transtraqueal. La técnica fue exitosa en el primer intento en los 10 casos. La anestesia regional y la sedación fueron suficientes, una vez que se observó estabilidad ventilatoria y hemodinámica, excepto en 1 caso donde se notaron taquicardia, hipertensión y agitación leve, sin comprometer el procedimiento y sin necesidad de intervención adicional. Nuestra serie de casos respalda la hipótesis de que la videolaringoscopia puede ser una alternativa a la intubación con fibra óptica en pacientes despiertos. Sugerimos que es más fácil de aprender y se puede realizar con un éxito, seguridad y comodidad similares para los pacientes.
-
Introduction
Tracheal intubation in patients with difficult airway continues to be one of the biggest challenges of anaesthesiologists. Awake tracheal intubation is recommended by many societies in patients with anticipated difficult airway[1],[2].
Awake fiberoptic intubation has for many years been the gold-standard in such situations. However, it is a technique with a demanding learning curve, unfamiliar to the routine of many anesthesiologists and the competence is difficult to maintain if rarely used[3],[4].
Videolaryngoscopy has already shown some advantages over direct laryngoscopy, particularly in patients with a difficult airway[5],[6]. Compared to fiberoptic intubation it uses a tech- nically simpler equipment and it is easier and quicker to learn. Anesthetists need around 10-18 intubations to be competent with fiberoptic intubation in anesthetised patients with normal airway[7],[8], being this number higher in awake patients with presumed difficult airway[4]. Only six intubations seem to be needed to reach the same level of competence with videolaryngoscopy[9]. Furthermore, there are no limitations to the tracheal tube diameter used and, if required, the size of the tracheal tube can be changed while maintaining the airway view. It also gives a wide visualization of structures, not being so impaired by blood or airway secretions. Finally, videolaryngoscopes and their maintenance are less expensive than fiberscopes, are portable (the availability of videolaryngoscopy devices in remote places can be managed much easier), faster and easier to set up, to clean and store. Most institutions still use standard fiber- scopes which require sterilization after each use; this process can delay the device’s availability for further use.
This article reports the successful tracheal intubation of 10 awake patients, by an anesthesiology resident, using the videolaryngoscope C-MAC®. The aim is to discuss awake videolaryngoscopy as an alternative to awake fibreoptic intubation and some practical aspects regarding sedation and regional anesthesia.
-
Material and Methods
We performed 10 tracheal intubations in awake adult patients admitted for elective surgery. Table 1 illustrate the demo- graphic data of patients.
All patients were informed about this approach and an informed consent was obtained. All parts of the procedure were explained and they were informed that they could immediately interrupt it just by raising one hand. They were aware that they could expect minimal discomfort, sensation of not flowing air, sensation of numbed and swollen tongue, some cough and possible vomiting.
A peripheral intravenous line was placed, a standard ASA monitoring and a nasal catheter with a flow of 4 L/min were applied. Administration of 0,5 mg atropine IV was performed before the procedure, in order to diminish airway secretions. Sedation with IV midazolam and alfentanil was provided, to reduced anxiety and airway reflexes and improve patient comfort, but without losing cooperation – the maintenance of verbal communication was used as a marker of a safe level of sedation.
Table 1. Demographic data of patients
| Gender | |
| Age, mean Male, n (%) Female, n (%) | 62,4
3 (30%) 7 (70%) |
| ASA score | |
| |
II III |
1 (10%)
7 (70%) 2 (20%) |
| Indication for awake intubation (2 out of 3) | |
| Mallampati III-IV
Reduced neck extensión Thyromental distance < 6 cm |
8
7 5 |
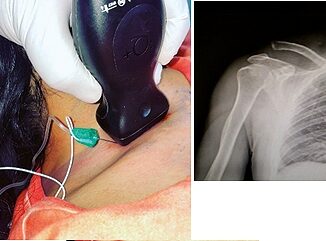
Topical anesthesia was achieved with puffs of 10% lidocaine spray applied on the surface of the tongue and oropharynges – each administration was synchronous with inspiration with the aim to reach as far as possible down the airway. Af- terwards, we used a 25G needle of 88 mm to perform a bilateral submucous block of the glossopharyngeal nerve, at the palatopharyngeal arch, with 1,5 + 1,5 mL of lidocaine 2% with adrenaline. Lastly, a transtracheal injection of 3 mL of lidocaine 2% was achieved.
Videolaryngoscopy was performed using the C-MAC® D- bladeTM. The device was gently introduced and a 7/7,5 tube was inserted with a stylet. After checking the cuff, the presence of capnography and pulmonary auscultation, a general anesthesia was induced.
-
Results
The patients of our report were all intubated by a first- year resident, already familiar with the use of the C-MAC® D- bladeTM” in anesthetised patients, and supervised by a senior anesthesiologist.
The technique was successful on the first attempt in the 10 cases, with low patient discomfort during the procedure. Regional anesthesia and sedation were sufficient, once ventilatory and hemodynamic stability was observed, except in 1 case where we noted tachycardia, hypertension and mild agitation, however without compromising the procedure and with no need for further intervention. We found some difficulty in performing the glossopharyngeal block in patients with a very big tongue. Three patients presented a small but limited local bleeding after the glossopharyngeal block.
-
Discussion
Videolaryngoscopy is increasing in popularity. Nonetheless, the use in awake intubations is relatively recent and there is still little evidence of its benefits. Some guidelines acknowledge vid- eolaryngoscopy as an alternative in that situations[2] and there are already randomized studies comparing videolaryngoscopy to awake fiberoptic tracheal intubation[10]-[17].
Most randomized studies found a significant shorter time to intubation with videolaryngoscope and none found difference in any other outcome, namely success rate, adverse events and patient satisfaction. Recorded time to intubation is initiated when the device is being introduced in the mouth until the tube is secured inside the trachea. If the time to set up all material was accounted the difference could be significantly bigger be- tween the two techniques.
Moreover, the intubations in these studies were all per- formed by anesthesiologists with expertise in both videolaryngoscopy and fibreoptic intubation. It has the advantage of ensuring superiority of one technique over the other. Though, since fibreoptic intubation is a more difficult technique to learn and to maintain expertise, our hypothesis is that the time of intubation would be bigger and even other outcomes could have different results if the intubations were performed by anesthesiologists with less experience. Cecilie H. Jepsen et al., performed a randomized trial comparing fiberoptic intubation or intubation with a videolaryngoscope in simulated difficult airway scenarios performed by residents with low experience with both, but with significant more experience with fibreoptic intubation[18]. The success of intubations with videolaryngos- copy was significantly better in 2 out of 3 scenarios, and in all 3 it was significantly faster. Finally, anesthesiologist stress could also be prevented when performing a technique that they are familiar with and adverse events could eventually be reduced.
Nevertheless, videolaryngoscopy has disadvantages, limitations and possible complications that we need to consider[19],[20]. It can’t be performed without an adequate mouth opening and is limited by a non-linear access to the glottis, re- quires a more cooperative patient, can provoke more serious traumatic injuries and is probably more stimulating and consequently more uncomfortable or worse to tolerate.
The choice of regional anesthesia was based on the fact that videolaryngoscopy exerts more traction on the tongue and upper airway, and therefore induces more gag reflex. The glos- sopharyngeal nerve is responsible for the sensory innervation of the pharynges and posterior third of the tongue. The trans- tracheal block produces topical anaesthesia secondary to direct contact of local anesthetic with mucosa. As the patient coughs during the injection, an extensive spread of local anaesthetic occurs and the sensory input from laryngeal and tracheal mucosa is blocked.
However, we acknowledge several limitations related to our report. It is a case series; therefore, we cannot demonstrate this technique’s superiority over other. Furthermore, our patients didn’t have a documented difficult airway or airway pathology; they had presumed difficult airway based on difficult airway predictors, all with a very low specificity.
In conclusion, there are still only a few studies comparing fiberoptic intubation to videolaryngoscopy in awake patients. None of them could demonstrate superiority of one technique over the other. However, most of the studies report videolaryngoscopy as an easier and faster technique to perform. Our cases series is not sufficient to take new conclusions, but it sug- gests the hypothesis that videolaryngoscopy can be an alterna- tive to fiberoptic intubation in awake patients. We also suggest it is easier to learn and can be performed with a similar success, security and comfort of patients. Being a more reflexogenic technique, we chose a regional anesthesia which, although more complex than just a topical anaesthesia, ensures patients comfort. More studies are necessary to recognize the rate of success, complications and differences in other outcomes be- tween techniques, so we can clarify the role of videolaryngoscopy in these situations.
Acknowledgments: The authors thank Ana Luísa Reina, licence in “Languages, literature and culture”, for language assistance.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
-
References
1. Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al.; American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013 Feb;118(2):251–70. https://doi.org/10.1097/ALN.0b013e31827773b2 PMID:23364566
2. Órfão J, Aguiar J, Carrilho A, et al. Consensos na Gestão Clínica da Via Aérea em Anestesiologia. Revista Da Sociedade Portuguesa De Anestesiologia 2016; 25(1): 7-31. https://doi.org/10.25751/rspa.8714 .
3. Marsland CP, Robinson BJ, Chitty CH, Guy BJ. Acquisition and maintenance of endoscopic skills: developing an endoscopic dexterity training system for anesthesiologists. J Clin Anesth. 2002 Dec;14(8):615–9. https://doi.org/10.1016/S0952-8180(02)00456-7 PMID:12565124
4. Kim H, So E, Karm MH, Kim HJ, Seo KS. Learning fiberoptic intubation for awake nasotracheal intubation. J Dent Anesth Pain Med. 2017 Dec;17(4):297–305. https://doi.org/10.17245/jdapm.2017.17.4.297 PMID:29349352
5. Lewis SR, Butler AR, Parker J, Cook TM, Schofield-Robinson OJ, Smith AF. Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation: a Cochrane Systematic Review. Br J Anaesth. 2017 Sep;119(3):369–83. https://doi.org/10.1093/bja/aex228 PMID:28969318
6. Pieters BM, Maas EH, Knape JT, van Zundert AA. Videolaryngoscopy vs. direct laryngoscopy use by experienced anaesthetists in patients with known difficult airways: a systematic review and meta-analysis. Anaesthesia. 2017 Dec;72(12):1532–41. https://doi.org/10.1111/anae.14057 PMID:28940354
7. Smith JE, Jackson AP, Hurdley J, Clifton PJ. Learning curves for fibreoptic nasotracheal intubation when using the endoscopic video camera. Anaesthesia. 1997 Feb;52(2):101–6. https://doi.org/10.1111/j.1365-2044.1997.23-az023.x PMID:9059089
8. Johnson C, Roberts JT. Clinical competence in the performance of fiberoptic laryngoscopy and endotracheal intubation: a study of resident instruction. J Clin Anesth. 1989;1(5):344–9. https://doi.org/10.1016/0952-8180(89)90073-1 PMID:2627408
9. Ray DC, Billington C, Kearns PK, Kirkbride R, Mackintosh K, Reeve CS, et al. A comparison of McGrath and Macintosh laryngoscopes in novice users: a manikin study. Anaesthesia. 2009 Nov;64(11):1207–10. https://doi.org/10.1111/j.1365-2044.2009.06061.x PMID:19825056
10. Abdellatif AA, Ali MA. GlideScope videolaryngoscope versus flexible fiberoptic bronchoscope for awake intubation of morbidly obese patient with predicted difficult intubation. Middle East J Anaesthesiol. 2014 Feb;22(4):385–92. PMID:25007692
11. Cohn AI, Zornow MH. Awake endotracheal intubation in patients with cervical spine disease: a comparison of the Bullard laryngoscope and the fiberoptic bronchoscope. Anesth Analg. 1995 Dec;81(6):1283–6. https://doi.org/10.1213/00000539-199512000-00027 PMID:7486117
12. Kramer A, Müller D, Pförtner R, Mohr C, Groeben H. Fibreoptic vs videolaryngoscopic (C-MAC(®) D-BLADE) nasal awake intubation under local anaesthesia. Anaesthesia. 2015 Apr;70(4):400–6. https://doi.org/10.1111/anae.13016 PMID:25764403
13. Mahran EA, Hassan ME. Comparative randomised study of GlideScope® video laryngoscope versus flexible fibre-optic bronchoscope for awake nasal intubation of oropharyngeal cancer patients with anticipated difficult intubation. Indian J Anaesth. 2016 Dec;60(12):936–8. https://doi.org/10.4103/0019-5049.195487 PMID:28003696
14. Mendonca C, Mesbah A, Velayudhan A, Danha R. A randomised clinical trial comparing the flexible fibrescope and the Pentax Airway Scope (AWS)(®) for awake oral tracheal intubation. Anaesthesia. 2016 Aug;71(8):908–14. https://doi.org/10.1111/anae.13516 PMID:27228959
15. Moore A, El-Bahrawy A, El-Mouallem E, Lattermann R, Hatzakorzian R, LiPishan W, et al. Videolaryngoscopy or fibreoptic bronchoscopy for awake intubation of bariatric patients with predicted difficult airways – a randomised, controlled trial. Anaesthesia. 2017 Apr;72(4):538–9. https://doi.org/10.1111/anae.13850 PMID:28297109
16. Rosenstock CV, Thøgersen B, Afshari A, Christensen AL, Eriksen C, Gätke MR. Awake fiberoptic or awake video laryngoscopic tracheal intubation in patients with anticipated difficult airway management: a randomized clinical trial. Anesthesiology. 2012 Jun;116(6):1210–6. https://doi.org/10.1097/ALN.0b013e318254d085 PMID:22487805
17. Wahba SS, Tammam TF, Saeed AM. Comparative study of awake endotracheal intubation with Glidescope video laryngoscope versus flexible fiber optic bronchoscope in patients with traumatic cervical spine injury. Egypt J Anaesth. 2012;28(4):257–60. https://doi.org/10.1016/j.egja.2012.05.002.
18. Jepsen CH, Gätke MR, Thøgersen B, Mollerup LT, Ruhnau B, Rewers M, et al. Tracheal intubation with a flexible fibreoptic scope or the McGrath videolaryngoscope in simulated difficult airway scenarios: a randomised controlled manikin study. Eur J Anaesthesiol. 2014 Mar;31(3):131–6. https://doi.org/10.1097/EJA.0b013e32836590a7 PMID:24145800
19. Cooper RM. Complications associated with the use of the GlideScope videolaryngoscope. Can J Anaesth. 2007 Jan;54(1):54–7. https://doi.org/10.1007/BF03021900 PMID:17197469
20. Magboul MM, Joel S. The video laryngoscopes, blind spots and retromolar trigonum injury by the GlideRite(®) rigid stylet. Anesth Essays Res. 2010;4(2):112–4. https://doi.org/10.4103/0259-1162.73519 PMID:25885242

 ORCID
ORCID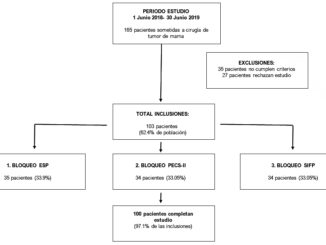

 Creative Commons Attribution
Creative Commons Attribution