María J. Andrade MD.2,*, Marcelino Murillo MD.1, María A. Zúñiga MD.2, Sebastián Amaya MD.2, Natalia Barreto MD.3, Carlos J. Castellanos3, Andres Felipe González MD.4
Recibido: 23-08-2022
Aceptado: 12-10-2022
©2023 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 52 Núm. 3 pp. 267-273|https://doi.org/10.25237/revchilanestv5207031447
PDF|ePub|RIS
Abstract
Background: Pediatric patients undergoing surgery under anesthesia may experience anxiety and distress during the perioperative period, for which benzodiazepines (BZD) can be employed as premedication in these scenarios. For this reason, it is important to highlight the pharmacological profile, use, and possible side effects in the pediatric perioperative population. Methods: Narrative Review using the Pubmed, Scopus and Embase databases for articles between 2000 and 2021 in English and Spanish using the keywords “Benzodiazepines”, “Pediatric Anesthesiology”, “Pharmacology”, “Adverse Effects”, and “Cerebral Apoptosis” Results: The principal side effects seen with BZD use in children mainly revolves around neurological manifestations, which include sedation, respiratory depression and prolonged awakening. There is evidence on the effectiveness of BZD in the pediatric population, which is used in a limited number of situations, such as surgical procedures that trigger acute anxiety. Conclusión: BZD has been widely studied in the literature, however it is important to highlight the possible complications and level of safety in the pediatric population. It has been evidenced that prolonged treatments not only increase the severity of neurodegeneration in the most vulnerable cerebral regions, but also trigger certain connectomic pathologies through wallerian and transneuronal degeneration.
Resumen
Antecedentes: Los pacientes pediátricos sometidos a cirugía bajo anestesia pueden experimentar ansiedad y angustia durante el período perioperatorio, por lo que las benzodiazepinas (BZD) pueden emplearse como premedicación en estos escenarios. Por ello, es importante destacar el perfil farmacológico, uso y posibles efectos secundarios en la población perioperatoria pediátrica. Métodos: Revisión narrativa utilizando las bases de datos Pubmed, Scopus y Embase para artículos entre 2000 y 2021 en inglés y español utilizando las palabras clave “Benzodiazepines”, “Pediatric Anesthesiology”, “Pharmacology”, “Adverse Effects” y “Cerebral Apoptosis” Resultados: Los principales efectos secundarios observados con el uso de BZD en niños giran principalmente entorno a las manifestaciones neurológicas, que incluyen sedación, depresión respiratoria y despertares prolongados. Existe evidencia sobre la efectividad de las BZD en la población pediátrica, que se utiliza en un número limitado de situaciones, como procedimientos quirúrgicos que desencadenan ansiedad aguda. Conclusión: Las BZD han sido ampliamente estudiadas en la literatura, sin embargo, es importante resaltar las posibles complicaciones y el nivel de seguridad en la población pediátrica. Se ha evidenciado que los tratamientos prolongados no solo aumentan la severidad de la neurodegeneración en las regiones cerebrales más vulnerables, sino que también desencadenan ciertas patologías conectómicas a través de la degeneración walleriana y transneuronal.
-
Introduction
Pediatric patients undergoing surgery under anesthesia may experience anxiety and distress during the perioperative period, for which benzodiazepines (BZD) can be employed as premedication. The main effects of BZD are sedation, hypnosis, decreased anxiety, anterograde amnesia, central muscle relaxation, and anticonvulsant activity[1],[2],[3].
Its mechanism of action is related to the inhibition of the polysynaptic pathway through direct interaction with gamma-aminobutyric acid (GABA) and ligand-gated modifiable chloride channels, acting on specific receptors in the central nervous system. These receptors are present in the fetus from the seventh week of gestation, enhancing neuronal inhibitory pathways mediated by GABA[4].
Side effects of BZD in children are mainly neurological[5], which include sedation, cognitive and psychomotor impairment, and compromise of complex skills. Pre-clinical data show that some BZDs can trigger accelerated apoptosis and other changes in the developing brain. The neuronal and oligodendrocyte apoptosis in the brain of neonates is generated by high plasma concentrations of BZD. Neuronal apoptosis is generated after an 8-hour exposure, with neurodegeneration notably increasing in severity proportionally to the time exposed[5],[6]. The period in which there is greater susceptibility to the neurological effect of BZD is from the third trimester of pregnancy to the third year of life[5]. The main objective of this narrative review is to study the pharmacological profile of BZDs, their uses, acceptable levels of sedation, and hemodynamic and adverse effects in the pediatric population, as well as comparing them with other types of medication described in the current literature.
-
Methodology
A narrative Review using the Pubmed, Scopus and Embase databases, searching for articles between 2000 and 2021 in English and Spanish using the keywords “Benzodiazepines”, “Pediatric Anesthesiology”, “Premedication”, “Pharmacology”, “Adverse Effects” and “Cerebral Apoptosis”. Articles were selected after a brief screening process by one of the authors who is a trained specialist in the field.
-
Pharmacokinetics and pharmacodynamics of benzodiazepines in children
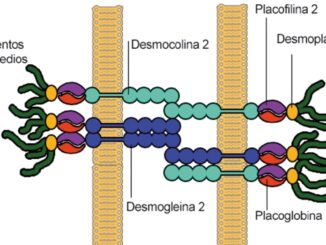
BZD act on specific receptors in the central nervous system. These receptors are present in the fetus from the seventh week of gestation, and enhance neuronal inhibitory pathways mediated by GABA[4]. Activation of the receptors causes an opening of chloride channels and passage to the cell, hyperpolarizing and stabilizing the postsynaptic membrane, therefore inhibiting transmission and neuronal activity. The GABA-A receptor is a pentameric protein that contains several binding sites called subunits, with the al and y2 subunits acting as receptor for BZDs, and the p subunit corresponding to barbiturates.
In the pediatric population, midazolam is preferred over other BZDs because of its high water solubility and rapid elimination. Its elimination half-life is significantly shorter than that of other BZD, but this is delayed in preterm infants compared with term infants and young children, which can be explained by the hepatic and renal immaturity of premature newborns, given that the expression of CPY is altered at birth but is subject to maturation in the first days of life[7].
BZDs are completely absorbed, with the exception of clorazepate, since it is first decarboxylated by gastric juice before its complete absorption. The metabolism is hepatic via cytochrome P450 into l-hydroxymidazolam, which is further metabolized in hydroxymidazolam glucuronide, which is excreted by the kidneys. Both metabolites are pharmacologically active and accumulation has been associated with the effect of prolonged sedation[8].
Midazolam is a highly specific substrate and is short-acting, and is generally administered as a one time dose or a continuous infusion in the intensive care unit (ICU), and has a dose de- pendent effect. The therapeutic window for midazolam is not well defined, but plasma concentrations of at least 0.1 mg/L are required, where levels above 2.4 mg/L are considered toxic[9]. The onset of action in pediatric patients is l0 minutes with a peak of action at 20-30 minutes, and dissipation of the effects 45 minutes after administration.
Intermediate and long-acting BZDs, such as diazepam, clorazepate and lorazepam, are less frequent since they interfere with the recovery and tend to have a prolonged pharmacological effect, generating prolonged sedation, since the half-life of these BZDs is l0 times greater than the half-life of midazolam.
Other BZDs such as oxazepam and lorazepam are metabolized by glucuronidation and have been considered a safe alter- native in patients with liver failure, but midazolam remains the first choice[10].
-
Favorable effects in anesthesia
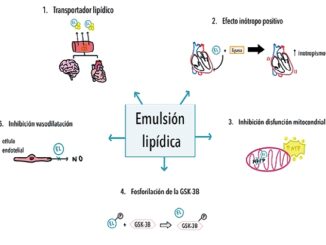
The main effects of BZDs are sedation, hypnosis, decreased anxiety, anterograde amnesia, central muscle relaxation, and anticonvulsant activity. In addition to their action on the central nervous system, BZDs have a dose-dependent ventilatory depressant effect and also cause a modest reduction in blood pressure and an increase in heart rate as a consequence of a decrease in systemic vascular resistance[ll],[l2],[l3].
Additionally, with respect to pharmacokinetic interactions, BZDs are given by their individual characteristics with respect to hepatic metabolism, which present phase I and phase II reactions during their biotransformation, which increases the risk of drug interactions. For example, the interaction between midazolam, morphine, and ketamine is additive; however, the inter- action between thiopental, propofol and other opioids (other than morphine) are synergistic due to the allosteric modulation of GABA-A receptors[2].
As an adjuvant, it significantly reduces the incidence of severe agitation on awakening after sevoflurane anesthesia after the administration of a single dose of 0.l mg/kg (midazolam). Midazolam, diazepam, and lorazepam are widely used for se- dation and, to some extent, also for induction and maintenance of anesthesia. Flumazenil is used as an antidote to sedation induced by BZDs[l3],[l4].
The intraoperative experience with BZDs has been studied together with other anesthetics, where it has been shown that BZDs reduces awareness compared to thiopental, ketamine,
and placebo[15]. It is also important to highlight the analgesic effects mediated by GABA-A receptors.
In cases where midazolam was added to lidocaine for intra- venous regional anesthesia, it was shown to improve the qual- ity of anesthesia and enhance intraoperative and postoperative analgesia without causing side effects[16].
In the pediatric setting, patients undergoing surgery un- der anesthesia may experience significant anxiety and distress during the perioperative period, however, BZDs may be used as premedication in these scenarios[1],[3],[17]. When comparing nasal spray and oral midazolam, it has been found that better sedation, easier induction, shorter recovery times, and post-an- esthetic recovery were evidenced in the nasal spray group over the oral group[17],[18].
In a study done by Banerjee et al., 90 patients between the age of 1 and 7 years were premedicated with different pharmacological regimens (Group M: Midazolam 0.5 mg/kg, Group K: Ketamine 6 mg/kg, and group C: Combination of ketamine 2.5 mg/kg and midazolam 0.25 mg/kg orally). It was concluded that the combination of low dose ketamine and midazolam (Group C) produced a satisfactory and quick onset of sedation, as well as a more rapid recovery when compared to Group M and K[19] Similarly, another study, that used the same medications (Group M: 0.5 mg/kg of oral midazolam, Group MK: 0.25 mg/kg of oral midazolam with 2.5 mg/kg of oral ketamine), showed that the combination of midazolam with ketamine al- lowed children to be calm and quiet while being awake, allowing for easier separation from parents[20].
Comparison of BZDs with clonidine for premedication has also shown to yield interesting results. A meta-analysis done by Dahmani et al., concluded that premedication with clonidine is superior to midazolam for producing sedation, and decreasing post-operative pain and emergence agitation[21]. A study done by Almenrader et al., organized 64 children randomly into 2 groups (Group M: 0.5 mg/kg of oral midazolam or Group C: 4 mcg/kg of oral clonidine) before mask induction. It was concluded that premedication with oral clonidine was superior to oral midazolam, since oral clonidine showed to be better accepted by the patients, produced more effective sedation, and showed better recovery from anesthesia[22].
Bayrak et al., conducted a study that compared midazolam to oral tramadol and nasal sufentanil. 60 children were randomized into 3 different groups (Group M: 0.5 mg/kg of midazolam in cherry juice, Group T: 3 mg/kg of tramadol drops, and Group S: 2 mcg/kg of intranasal sufentanil), and concluded that intranasal sufentanil and oral midazolam are more appropriate than tramadol drops for premedication in children[23]. A similar study done by Howell et al., compared oral transmucosal fentanyl and oral midazolam for premedication in pediatric patients. 80 children between 3-9 years of age were randomly assigned to receive either 2.5 mL of oral transmucosal fentanyl in lollipop format with 0.5 mL/kg placebo syrup, or midazolam syrup (0.5 mg/kg) with a placebo lollipop. It was concluded that oral transmucosal fentanyl citrate was as effective as midazolam in allowing anesthesia compliance, had better appeal in children, and better emergence characteristics[24].
Many studies have shown that dexmedetomidine is also comparable, if not superior to midazolam in the premedication context. Yuen et al., conducted a study with 96 children randomly separated into different groups (Group M: 0.5 mg/kg of midazolam in acetaminophen syrup and intranasal placebo, Group D0.5: 0.5 mcg/kg of intranasal dexmedetomidine with acetaminophen cough syrup, and Group D1: 1 mcg/kg of intranasal dexmedetomidine with acetaminophen cough syrup. There was no significant difference between parental separation acceptance between the groups, and the authors concluded that intranasal dexmedetomidine produces more sedation than oral midazolam, but with similar patient cooperation[25]. A meta-analysis done by Sun et al., on if dexmedetomidine is superior to midazolam concluded that dexmedetomidine pre- medication is superior to midazolam in the context of producing sedation upon parent separation, as well as mask acceptance. Dexmedetomidine also boasts benefits such as reducing requirements for rescue analgesia and a decrease in risk for agitation and/or delirium in the postoperative period[26]. Similarly, another meta-analysis done by Pasin et al., found that dexmedetomidine is effective in decreasing anxiety during patient separation from parents, as well as a decrease in postoperative agitation, and a more effective postoperative analgesia when compared to midazolam[27].
Melatonin and other sleep-inducing agents have also been studied and compared to midazolam for premedication. A study done by Gitto et al., compared midazolam to melatonin in patients between the ages of 5 and 14 years old, who were randomly assigned to a group (oral melatonin 0.5 mg/kg or oral midazolam 0.5 mg/kg, both with a maximum dose of 20 mg). The study concluded that melatonin enhances the potency of propofol, and that it was equally as effective as midazolam in the context of sedation (28). Another study done by Impellizzeri et al., randomly assigned pediatric patients to different groups (oral midazolam 0.5 mg/kg or oral melatonin 0.5 mg/kg, both with a maximum dose of 20 mg). The authors concluded that melatonin was as effective as midazolam in decreasing anxiety in both the preoperative room and during anesthesia induction[29]. A study with another sleep agent, zolpidem, was carried out by Hanna et al., with 80 patients between the ages of 2 and 9 years old, who were randomly assigned to different groups (midazolam 0.5 mg/kg or zolpidem 0.25 mg/kg orally). The study concluded that zolpidem at the dosage used in the trial, was similar to midazolam in regard to anxiety scoring, but inferior with regard to mask acceptance[30].
As an alternative, different adjuvant mixtures of drugs widely used in the perioperative period have been created such as remimazolam, which is an ultrashort-acting intravenous sedative/anesthetic plus BZD combination, with possible uses in induction and maintenance of general anesthesia[31]. Remimazolam was shown to be safe to use for general anesthesia in pediatric patients, because it does not produce injection site pain, which is common in propofol use, and there are reports that general anesthesia with remimazolam has been safely per- formed in other high-risk patients[32].
In addition to remimazolam, midazolam is also used for pediatric patients who require anesthesia/sedation for procedures. It has been shown to be an effective BZD for minimal or moderate sedation in children aged 4 months to 18 years, with dosage ranging between 0.25 to 1.5 mg/kg, however, increasing the dose increases the probability of adverse events such as paradoxical reactions, respiratory events and excessive sedation[33]. A systematic review concluded that intranasal midazolam produces effective sedation for the suture of traumatic
lacerations at doses of 0.2-0.5 mg/kg, and does not produce significant adverse effects or require prolonged recovery[34].
Ketamine is also used for sedation/analgesia, standing out for its rapid action, short duration, adequate safety profile, possible administration by almost any route, and sedoanalgesia effectiveness[35]. Midazolam can be used in combination with ketamine; a study by Acworth et al., studied 53 pediatric patients who were randomized into groups that received intranasal midazolam (INM) (0.4 mg/kg) or intravenous ketamine (1 mg/kg) plus intravenous midazolam (0.1 mg/kg), and it was concluded that the combination is superior to INM in terms of speed of onset of sedation (5.3 minutes faster) and consistency of effect (mean sedation scores and the significantly higher visual analog sedation scale scores for the combination). In addition, pediatric patients given intravenous ketamine plus intra- venous midazolam were discharged 19 minutes faster.
Dexmedetomidine is also an alternative for sedation/analgesia in pediatric patients, which is of greater benefit in cases of children with neurological deterioration or in those who do not tolerate BZDs[36]. A systematic review and meta-analysis of randomized clinical trials conducted by Lin Y et al., compared dexmedetomidine with other sedation methods, including midazolam, and showed that dexmedetomidine compared to midazolam has a lower incidence of respiratory depression or desaturation, a higher rate of success in sedation, but with a higher incidence rate of bradycardia[37]. Another systematic review and meta-analysis of randomized controlled trials (Kim HJ, et al) also indicates that dexmedetomidine has sedative efficacy similar to intranasal midazolam without producing respiratory depressant effects[38].
There are many presentations and dosing schemes that can be used according to the age of the pediatric patient. Between the age of 1 month and 18 years of age, oral midazolam (2.5 mg/mL) solution can be used at a dose of 0.25 mg/kg, with a maximum dose of 20 mg. Similarly, for patients between 6 months and 18 years of age, buccal midazolam (10 mg/mL) can be used at a recommended dose of 0.3 mg/kg, with a maxi- mum dose of 10 mg. For patients between the ages of 12 to 18 years, 10 mg temazepam tablets or 2 mg/mL solution can be used, with a suggested dose of 10-20 mg[39].
-
Side effects
Among the most frequent side effects is iatrogenic withdrawal, which is described mainly in the critically ill pediatric population. As such, this side effect is relatively frequent in the pediatric and adult intensive care population who were subject- ed to opioids and/or BZD on a regular basis for a period great- er than or equal to 72 hours. There have been certain studies which found an independent association between younger age (range 2 weeks to 6 months of age) with increased abstinence. Therefore, the younger the patient, the greater the risk of withdrawal, which may vary over time, especially due to the immaturity of the receptors (GABA, NMDA, and opioid receptors) [40]. Abstinence and dependence have raised special concern and even controversy due to the rise in their incidence[12], with patterns that follow withdrawal varying widely. BZDs are also drugs of abuse, either alone or in conjunction with opioids and stimulants. It has been claimed that the use of these drugs are associated with increased mortality[12].
Within the literature, various strategies have been proposed to prevent the appearance of tolerance and withdrawal, all reaching the same objective which is the administration of the least amount of sedative or analgesic drugs for the shortest possible time. To achieve this, there are various tools validated for the level of analgosedation of pediatric patients admit- ted to the ICU. For example, a particular strategy focuses on avoiding weaning greater than a daily reduction of 20% with respect to the initial dose[41]. In 2018, the Sophia Observation Symptoms-Pediatric Delirium (SOS-PD) scale was derived from the Sophia Observation Withdrawal Symptoms (SOS) scale; to monitor withdrawal syndrome with a single tool. This scale can be applied to children older than 3 months by any health personnel, allowing for continuous control and prevention of this adverse effect[42].
Some of the other frequent adverse effects are central nervous system depression, impaired psychomotor performance, amnesia, respiratory depression, and the potential for dependence and abuse[42]. It is important to bear in mind that its pharmacological action is exerted from the binding to type A GABA related chloride receptors in the central nervous system, producing an increase in its inhibitory action leading to relaxation and producing anterograde amnesia.
In regard to the management and treatment of these secondary reactions to BZDs, it is important to control the airway, and employ proper monitoring of blood pressure. Within the literature, certain studies consider that some side effects can be mitigated with pharmacological management using physostigmine, flumazenil and haloperidol[43]. To understand the adverse effects, it is important to take into account that the vast majority of pre-clinical data show that some of these agents can trigger accelerated apoptosis and other changes in the developing brain[5].
During development, excess neurons are eliminated through apoptosis and neuronal survival depends clearly on their activity, and in the same way, dendritic and synaptic development is linked to this activity. An explanation for this phenomenon of neuronal apoptosis would be that the changes are related to the neuronal activity induced by anesthesia[5]. In the developing brain, BZD can cause neuronal and oligodendroglial apoptosis, alter synaptogenesis, inhibit neurogenesis, and trigger long-term neurocognitive sequelae. In humans, the vulnerable period is expected to extend from the third trimester of pregnancy to the third year of life[5].
The neuronal and oligodendrocyte apoptosis in the brain of neonates is generated by high plasma concentrations of BZD. Specifically, neurodegeneration will notably increase in severity proportionally to the time exposed. Oligodendroglial apoptosis is said to show an early peak at 8 hours with a subsequent descending rate at 36 hours. In the case of longer exposures, the neuro-apoptotic process leads to axon degeneration and expansion, generating involvement of trans-neuronal targets within interconnected brain regions[6].
It is also plausible that drugs that alter neuronal activity have some impact on the number and morphology of neuronal cells, since GABA, N-methyl-d-aspartate (NMDA) and opioid receptors also they have a direct role in neuronal migration, differentiation and maturation[5].
In the literature it has been described that before the ad- ministration of BZDs, some patients, instead of experiencing sedation, present a reaction characterized by emotional dis- inhibition, psychomotor agitation and even aggressiveness. This phenomenon, which in most cases is idiosyncratic, is difficult to predict and is more common in the elderly population[44],[45],[46]. However, this paradoxical reaction is relatively uncommon, occurring in approximately less than 1% of patients[46]. It is important to know that there are some causal factors identified. Some evidence suggests that these reactions may occur secondary to advanced age, a genetic link, a history of alcohol abuse, or psychological disorders. Another theory is that the inhibitory action of BZDs can cause arousal by generating loss of cortical immobilization in some patients. Addition- ally, BZDs reduce serotonin neurotransmission, so a decrease in serotonin concentrations can precipitate aggressive behavior[47],[48]. Another theory about this paradoxical reaction is the pharmacokinetic variability that a person could present secondary to a genetic link, given a reflection of the genetically determined variability in the density of the BZD receptor throughout the brain[48]. It has been theorized that these sub- groups of patients have altered pharmacodynamic response to BZDs; however, the exact differences have not been specifically characterized in the literature[47].
In a cross-sectional observational study in Chile in 2021, the risk factors for paradoxical reaction associated with intra- venous sedation with midazolam were evaluated, and it was determined that the vast majority of reactions are mild and manageable with simple measures, and most do not require drug therapy[49]. Treatment of paradoxical reactions secondary to BZDs is largely considered supportive management, with airway and blood pressure control. Additionally, a limited number of case studies report the use of physostigmine, flumazenil, and haloperidol[47]. Among these medications, flumazenil, a BZD antagonist, has been shown to control these reactions successfully with minimal adverse effects. Reversal of sedation in pediatric patients at least 1 year of age can be achieved with an initial dose of flumazenil of 0.01 mg/kg (up to 0.2 mg) intravenously over 15 seconds. Maintenance doses of 0.01 mg/ kg (up to 0.2 mg) can be administered repeatedly to achieve the desired level of consciousness, keeping in mind that the maximum recommended dose of flumazenil in children is 0.05 mg/kg or 1.0 mg[47].
On the other hand, physostigmine was the first agent used to control paradoxical reactions to BZDs. By easily crossing the blood-brain barrier, the drug increases cholinergic stimulation and can reverse drug-induced central nervous system depression[47].
Based on the above, it can be concluded that prolonged treatments not only increase the severity of neurodegeneration in the most vulnerable regions, but also trigger certain connectomic pathologies through wallerian and transneuronal degeneration[6].
-
Conclusion
BZDs have been widely studied in the literature, however it is important to highlight the possible complications and level of safety in the pediatric population. It has been evidenced that prolonged treatments not only increase the severity of neuro- degeneration in the most vulnerable cerebral regions, but also trigger certain connectomic pathologies through wallerian and transneuronal degeneration.
-
Referencias
1. Bergendahl H, Lönnqvist PA, Eksborg S. Clonidine in paediatric anaesthesia: review of the literature and comparison with benzodiazepines for premedication. Acta Anaesthesiol Scand. 2006 Feb;50(2):135–43. https://doi.org/10.1111/j.1399-6576.2006.00940.x PMID:16430532
2. Cornett EM, Novitch MB, Brunk AJ, Davidson KS, Menard BL, Urman RD, et al. New benzodiazepines for sedation. Best Pract Res Clin Anaesthesiol. 2018 Jun;32(2):149–64. https://doi.org/10.1016/j.bpa.2018.06.007 PMID:30322456
3. Verma RK, Paswan A, De A, Gupta S. Premedication with midazolam nasal spray: an alternative to oral midazolam in children. Anesth Pain Med. 2012;1(4):248–51. https://doi.org/10.5812/aapm.4567 PMID:24904809
4. Ng E, Taddio A, Ohlsson A. Intravenous midazolam infusion for sedation of infants in the neonatal intensive care unit. Cochrane Database Syst Rev. 2017 Jan;1(1):CD002052. https://doi.org/10.1002/14651858.CD002052.pub3 PMID:28141899
5. Davidson A, Flick RP. Neurodevelopmental implications of the use of sedation and analgesia in neonates. Clin Perinatol. 2013 Sep;40(3):559–73. https://doi.org/10.1016/j.clp.2013.05.009 PMID:23972757
6. Noguchi KK, Fuhler NA, Wang SH, Capuano S 3rd, Brunner KR, Larson S, et al. Brain pathology caused in the neonatal macaque by short and prolonged exposures to anticonvulsant drugs. Neurobiol Dis. 2021 Feb;149:105245. https://doi.org/10.1016/j.nbd.2020.105245 PMID:33385515
7. Donato J, Rao K, Lewis T. Pharmacology of Common Analgesic and Sedative Drugs Used in the Neonatal Intensive Care Unit. Clinics in Perinatology [Internet]. 2019 Dec;46(4):673–92. https://doi.org/10.1016/j.clp.2019.08.004.
8. van Groen BD, Krekels EH, Mooij MG, van Duijn E, Vaes WH, Windhorst AD, et al. The Oral Bioavailability and Metabolism of Midazolam in Stable Critically Ill Children: A Pharmacokinetic Microtracing Study. Clin Pharmacol Ther. 2021 Jan;109(1):140–9. Available from: https://doi-org.ezproxy.unbosque.edu.co/10.1002/cpt.1890 https://doi.org/10.1002/cpt.1890 PMID:32403162
9. Favié LM, Groenendaal F, van den Broek MP, Rademaker CM, de Haan TR, van Straaten HL, et al.; on behalf of the PharmaCool study group. Phenobarbital, Midazolam Pharmacokinetics, Effectiveness, and Drug-Drug Interaction in Asphyxiated Neonates Undergoing Therapeutic Hypothermia. Neonatology. 2019;116(2):154–62. https://doi.org/10.1159/000499330 PMID:31256150
10. Royston D, Hemmings HC. Physiology and Pharmacology for Anesthesia: Foundations and Clinical Application: Expert Consult-Online and Print. Elsevier; 2013.
11. Olkkola, K. T., & Ahonen, J. (2008). Midazolam and other benzodiazepines. Modern anesthetics, 335-360. https://doi.org/10.1007/978-3-540-74806-9_16.
12. Lader M. Benzodiazepine harm: how can it be reduced? Br J Clin Pharmacol. 2014 Feb;77(2):295–301. https://doi.org/10.1111/j.1365-2125.2012.04418.x PMID:22882333
13. Gallagher C. Benzodiazepines: sedation and Agitation. Dent Update. 2016;43(1):83–6. https://doi.org/10.12968/denu.2016.43.1.83 PMID:27024905
14. Kawai M, Kurata S, Sanuki T, Mishima G, Kiriishi K, Watanabe T, et al. The effect of midazolam administration for the prevention of emergence agitation in pediatric patients with extreme fear and non-cooperation undergoing dental treatment under sevoflurane anesthesia, a double-blind, randomized study. Drug Des Devel Ther. 2019 May;13:1729–37. https://doi.org/10.2147/DDDT.S198123 PMID:31190751
15. Messina AG, Wang M, Ward MJ, Wilker CC, Smith BB, Vezina DP, et al. Anaesthetic interventions for prevention of awareness during surgery. Cochrane Database Syst Rev. 2016 Oct;10(10):CD007272. https://doi.org/10.1002/14651858.CD007272.pub2 PMID:27755648
16. Farouk S, Aly A. Quality of lidocaine analgesia with and without midazolam for intravenous regional anesthesia. J Anesth. 2010 Dec;24(6):864–8. https://doi.org/10.1007/s00540-010-1015-1 PMID:20830491
17. Manoj M, Satya Prakash MV, Swaminathan S, Kamaladevi RK. Comparison of ease of administration of intranasal midazolam spray and oral midazolam syrup by parents as premedication to children undergoing elective surgery. J Anesth. 2017 Jun;31(3):351–7. https://doi.org/10.1007/s00540-017-2330-6 PMID:28271228
18. Deshmukh PV, Kulkarni SS, Parchandekar MK, Sikchi SP. Comparison of preanesthetic sedation in pediatric patients with oral and intranasal midazolam. J Anaesthesiol Clin Pharmacol. 2016;32(3):353–8. https://doi.org/10.4103/0970-9185.168205 PMID:27625485
19. Banerjee B, Bose A, Pahari S, Dan AK. A comparative study of paediatric oral premedication: midazolam, ketamine and low dose combination of midazolam and ketamine. J Indian Med Assoc. 2011 Jun;109(6):386–8. PMID:22315765
20. Ghai B, Grandhe RP, Kumar A, Chari P. Comparative evaluation of midazolam and ketamine with midazolam alone as oral premedication. Paediatr Anaesth. 2005 Jul;15(7):554–9. https://doi.org/10.1111/j.1460-9592.2004.01523.x PMID:15960638
21. Dahmani S, Brasher C, Stany I, Golmard J, Skhiri A, Bruneau B, et al. Premedication with clonidine is superior to benzodiazepines. A meta analysis of published studies. Acta Anaesthesiol Scand. 2010 Apr;54(4):397–402. https://doi.org/10.1111/j.1399-6576.2009.02207.x PMID:20085541
22. Almenrader N, Passariello M, Coccetti B, Haiberger R, Pietropaoli P. Premedication in children: a comparison of oral midazolam and oral clonidine. Paediatr Anaesth. 2007 Dec;17(12):1143–9. https://doi.org/10.1111/j.1460-9592.2007.02332.x PMID:17986032
23. Bayrak F, Gunday I, Memis D, Turan A. A comparison of oral midazolam, oral tramadol, and intranasal sufentanil premedication in pediatric patients. J Opioid Manag. 2007;3(2):74–8. https://doi.org/10.5055/jom.2007.0043 PMID:17520986
24. Howell TK, Smith S, Rushman SC, Walker RW, Radivan F. A comparison of oral transmucosal fentanyl and oral midazolam for premedication in children. Anaesthesia. 2002 Aug;57(8):798–805. https://doi.org/10.1046/j.1365-2044.2002.02698_4.x PMID:12133094
25. Yuen VM, Hui TW, Irwin MG, Yuen MK. A comparison of intranasal dexmedetomidine and oral midazolam for premedication in pediatric anesthesia: a double-blinded randomized controlled trial. Anesth Analg. 2008 Jun;106(6):1715–21. https://doi.org/10.1213/ane.0b013e31816c8929 PMID:18499600
26. Sun Y, Lu Y, Huang Y, Jiang H. Is dexmedetomidine superior to midazolam as a premedication in children? A meta-analysis of randomized controlled trials. Paediatr Anaesth. 2014 Aug;24(8):863–74. https://doi.org/10.1111/pan.12391 PMID:24666837
27. Pasin L, Febres D, Testa V, Frati E, Borghi G, Landoni G, et al. Dexmedetomidine vs midazolam as preanesthetic medication in children: a meta-analysis of randomized controlled trials. Paediatr Anaesth. 2015 May;25(5):468–76. https://doi.org/10.1111/pan.12587 PMID:25559766
28. Gitto E, Marseglia L, D’Angelo G, Manti S, Crisafi C, Montalto AS, et al. Melatonin versus midazolam premedication in children undergoing surgery: A pilot study. J Paediatr Child Health. 2016 Mar;52(3):291–5. https://doi.org/10.1111/jpc.13007 PMID:26515269
29. Impellizzeri P, Vinci E, Gugliandolo MC, Cuzzocrea F, Larcan R, Russo T, et al. Premedication with melatonin vs midazolam: efficacy on anxiety and compliance in paediatric surgical patients. Eur J Pediatr. 2017 Jul;176(7):947–53. https://doi.org/10.1007/s00431-017-2933-9 PMID:28540436
30. Hanna AH, Ramsingh D, Sullivan-Lewis W, Cano S, Leiter P, Wallace D, et al. A comparison of midazolam and zolpidem as oral premedication in children, a prospective randomized double-blinded clinical trial. Paediatr Anaesth. 2018 Dec;28(12):1109–15. https://doi.org/10.1111/pan.13501 PMID:30328648
31. Keam SJ. Remimazolam: first Approval. Drugs. 2020 Apr;80(6):625–33. https://doi.org/10.1007/s40265-020-01299-8 PMID:32274703
32. Horikoshi Y, Kuratani N, Tateno K, Hoshijima H, Nakamura T, Mieda T, et al. Anesthetic management with remimazolam for a pediatric patient with Duchenne muscular dystrophy. Medicine (Baltimore). 2021 Dec;100(49):e28209. https://doi.org/10.1097/MD.0000000000028209 PMID:34889305
33. Manso MA, Guittet C, Vandenhende F, Granier LA. Efficacy of oral midazolam for minimal and moderate sedation in pediatric patients: A systematic review. Paediatr Anaesth. 2019 Nov;29(11):1094–106. https://doi.org/10.1111/pan.13747 PMID:31538393
34. Gómez-Manzano FJ, Laredo-Aguilera JA, Cobo-Cuenca AI, Rabanales-Sotos J, Rodríguez-Cañamero S, Martín-Espinosa N, et al. Evaluation of Intranasal Midazolam for Pediatric Sedation during the Suturing of Traumatic Lacerations: A Systematic Review. Children (Basel). 2022 Apr;9(5):644. https://doi.org/10.3390/children9050644 PMID:35626821
35. Simonini A, Brogi E, Cascella M, Vittori A. Advantages of ketamine in pediatric anesthesia. Open Med (Wars). 2022 Jul;17(1):1134–47. https://doi.org/10.1515/med-2022-0509 PMID:35859796
36. Buck ML. Dexmedetomidine use in pediatric intensive care and procedural sedation. J Pediatr Pharmacol Ther. 2010 Jan;15(1):17–29. https://doi.org/10.5863/1551-6776-15.1.17 PMID:22477789
37. Lin Y, Zhang R, Shen W, Chen Q, Zhu Y, Li J, et al. Dexmedetomidine versus other sedatives for non-painful pediatric examinations: A systematic review and meta-analysis of randomized controlled trials. J Clin Anesth. 2020 Jun;62:109736. https://doi.org/10.1016/j.jclinane.2020.109736 PMID:32018129
38. Kim HJ, Shin WJ, Park S, Ahn HS, Oh JH. The sedative effects of the intranasal administration of dexmedetomidine in children undergoing surgeries compared to other sedation methods: A systematic review and meta-analysis. J Clin Anesth. 2017 May;38:33–9. https://doi.org/10.1016/j.jclinane.2017.01.014 PMID:28372674
39. Heikal S, Stuart G. Anxiolytic premedication for children. BJA Educ. 2020 Jul;20(7):220–5. https://doi.org/10.1016/j.bjae.2020.02.006 PMID:33456954
40. Hudak ML, Tan RC, Frattarelli DA, Galinkin JL, Green TP, Neville KA, et al.; COMMITTEE ON DRUGS; COMMITTEE ON FETUS AND NEWBORN; American Academy of Pediatrics. Neonatal drug withdrawal. Pediatrics. 2012 Feb;129(2):e540–60. https://doi.org/10.1542/peds.2011-3212 PMID:22291123
41. Amigoni A, Conti G, Conio A, Corno M, Fazio PC, Ferrero F, et al. Recommendations for analgesia and sedation in critically ill children admitted to intensive care unit. Journal of Anesthesia, Analgesia and Critical Care [Internet]. 2022 Feb 12;2(1). https://doi.org/10.1186/s44158-022-00036-9.
42. Ista E, Te Beest H, van Rosmalen J, de Hoog M, Tibboel D, van Beusekom B, et al. Sophia Observation withdrawal Symptoms-Paediatric Delirium scale: A tool for early screening of delirium in the PICU. Aust Crit Care. 2018 Sep;31(5):266–73. https://doi.org/10.1016/j.aucc.2017.07.006 PMID:28843537
43. Duceppe MA, Perreault MM, Frenette AJ, Burry LD, Rico P, Lavoie A, et al. Frequency, risk factors and symptomatology of iatrogenic withdrawal from opioids and benzodiazepines in critically Ill neonates, children and adults: A systematic review of clinical studies. J Clin Pharm Ther. 2018; https://doi.org/10.1111/jcpt.12787 PMID:30569508
44. Lichtfield NB. Complications of intravenous diazepam-Adverse psychological reactions. (An assessment of 16,000 cases). Anesth Prog. •••;27(6):175–83.
45. García S, rodríguez J, Sievers P. Efecto de la sedación en el desarrollo de delirium en pacientes adultos mayores sometidos a cirugía con anestesia espinal. Estudio clíni- co prospectivo. rev Chil Anest. 2012,41:124-7.
46. Barrionuevo L, Correa K, Consiglio M. Incidencia de reacciones adversas en sedación con midazolam endo-venoso o intramuscular en niños jóvenes en situación de discapacidad. Experiencia de dos años. rehabil. integral; 13 (1): 8-13.
47. Mancuso CE, Tanzi MG, Gabay M. Paradoxical reactions to benzodiazepines: literature review and treatment options. Pharmacotherapy. 2004 Sep;24(9):1177–85. https://doi.org/10.1592/phco.24.13.1177.38089 PMID:15460178
48. Moon YE. Paradoxical reaction to midazolam in children. Korean J Anesthesiol. 2013 Jul;65(1):2–3. https://doi.org/10.4097/kjae.2013.65.1.2 PMID:23904931
49. Estefó Magdalena, Ojeda Dagoberto, Cisternas Patricia, Arraño Nicolás, Zanetta Hugo. Factores de riesgo de reacción paradójica asociados a sedación endovenosa con midazolam. Rev. Med. Chile [Internet]. 2021 Feb [citado 2022 Ago 12]; 149 (2) : 237-241.

 ORCID
ORCID