Enrique Sepúlveda Haro1,*, Jaime Torres Varona1, Salvador Romero Molina1, Juan Manuel Cañero Ávila1
Recibido: 06-07-2022
Aceptado: 10-10-2022
©2023 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 52 Núm. 1 pp. 110-112|https://doi.org/10.25237/revchilanestv5210111510
PDF|ePub|RIS
Bloqueo de la vaina de los rectos bilateral como única técnica anestésica para reparación quirúrgica urgente de hernia umbilical incarcerada
Abstract
Rectus sheath block is an interesting analgesic technique for umbilical hernia repair and there are some case reports where it was even used as the sole anesthetic. We describe the clinical case of a patient who required an urgent surgery for an incarcerated umbilical hernia and who was successfully managed with a bilateral rectus sheath block along with light sedation. Ultrasound-guided bilateral rectus sheath block provided anesthesia for our patient, avoiding the risks of the general and spinal anesthesia for his particular clinical situation and achieving an excellent postoperative analgesia, a fast recovery and hospital discharge without any complications.
Resumen
El bloqueo de la vaina de los rectos es una técnica analgésica interesante para la reparación de la hernia umbilical y hay casos descritos donde incluso se ha usado como único anestésico. Describimos el caso clínico de un paciente que precisó reparación urgente de una hernia umbilical incarcerada y que fue manejado con éxito con un bloqueo de la vaina de los rectos bilateral junto con sedación ligera. El bloqueo ecoguiado de la vaina de los rectos bilateral aportó anestesia quirúrgica para nuestro paciente, evitando los riesgos de la anestesia general y espinal en su peculiar situación clínica y consiguió una analgesia postoperatoria excelente, una rápida recuperación y alta hospitalaria sin complicaciones.
-
Introduction
An umbilical hernia is the protrusion of intra-abdominal contents through a defect in the abdominal muscles situated at or near the umbilicus. Among the different analgesic techniques performed for umbilical hernia repair stands out the rectus sheath block (RSB). This is a fascial block that provides analgesia for somatic pain at the midline of the abdominal wall between the xiphoid process and the pubis symphysis. Schleich described this block in 1899 to achieve abdominal muscle relaxation in adults[1], although its useful analgesic effect for umbilical hernia repair was noted by Ferguson later in 1996[2].
This technique aims to block the nerve conduction at the terminal branches of the T9-T11 thoracoabdominal nerves, the ones that innervate the umbilical region. These nerves travel anteriorly between the transverse abdominis muscle and the internal abdominal oblique muscle. They perforate the posterior layer of the internal abdominal oblique muscle’s aponeurosis and reach the virtual space between the rectus abdominis muscle and its posterior fascia, where the anesthetic solution is de- posited[3]. This fascial block is effective and, when performed under ultrasound guidance, it is a safe technique[4].
We describe the clinical case of a patient who required an urgent surgery for an incarcerated umbilical hernia and who was successfully managed with RSB along with light sedation.
-
Clinical case
A male patient, 79 years old, 80 kg, 172 cm, with an incarcerated umbilical hernia containing part of the greater omentum was assessed for urgent surgery. He had hypertension, dyslipidemia, permanent atrial fibrillation, left hemispheric ischemic stroke and was treated with rivaroxaban, omeprazol, bisoprolol, ramipril, furosemide and tamsulosin. He had received no previous surgeries.
The incarcerated umbilical hernia had a 10 mm diameter defect and a 4,6 x 2,6 cm hernial sac containing part of the greater omentum’s adipose tissue showing radiologic signs of inflammation and cellulitis of the adjacent abdominal wall (Figure 1).
The patient had fastened for 12 hours but the CT scan showed a great amount of gastric content. The last rivaroxaban dose was administered 24 hours before. The biochemical analysis, hemogram, clotting test and chest radiograph were normal. He presented a limited mouth opening and a Mallampati class III airway.
Standard monitorization, peripheral vein cannulation and oxygen supplementation with nasal cannula were applied. A superficial level of sedation was achieved with intravenous midazolam 2 mg and a Minto model target-controlled-infusion remifentanil between 1-2 ng/ml. Then, an ultrasound-guided bilateral rectus sheath block was performed (Locoplex 50 mm, 20G, Vygon; 13-6 MHz linear transducer, SonoSite SII, Fujifilm, Bothell, WA, USA) with levobupivacaine 0.25%, 30 ml each side. We also set up the drugs, suctioning, and airway instrumental for any necessary conversion to general anesthesia, and 10 minutes later the surgery started. Intravenous dexamethasone 8 mg, metamizol 2 g, paracetamol 1 g and ondansetron 4 mg were administered.
After an elliptical left lateral umbilical incision, dissection of the hernial orifice and sac was performed. The hernial sac was opened and the congested omentum was ligated and sectioned. Finally, the hernial defect was closed with a continuous suture, the umbilicus was reinserted, the subcutaneous tissue was sutured, and the skin was closed with surgical staples.
The surgery was performed uneventfully, with good patient collaboration along with respiratory and hemodynamic stability. Section of the omentum did not produce any pain. Near the end of the procedure, the patient suffered a brief disorientation episode with arms shaking that ceased with a bolus of propofol 20 mg.
The procedure lasted for 30 minutes, then the patient spent 60 minutes in the Post-Anesthesia Care Unit, was transferred to the ward without any pain and was later discharged home 12 hours after the surgery without any complications.
-
Discussion
An incarcerated umbilical hernia is a surgical emergency. It can be managed with different anesthetic techniques and the most frequently used are general anesthesia (GA) and spinal anesthesia. General anesthesia associated risks should be al- ways considered, and our patient was at high risk: emergency surgery, obesity, acute abdomen and gastric content observed in the CT scan[5].
Neuraxial anesthesia is contraindicated in the presence of coagulopathy. Rivaroxaban, a direct oral anticoagulant, should be stopped for a minimum of 48 hours in the absence of kidney failure before performing these anesthetic techniques which are considered at high bleeding risk. Our patient had stopped the drug for 24 hours, which was long enough to perform the surgery, considered at low bleeding risk. Reversion of the anti- coagulant effect of rivaroxaban was dismissed because of the moderate risk of thromboembolic events of the patient, who had suffered from an ischemic stroke (> 3 months)[6].
In our clinical case, a thorough benefit-risk balance regarding the anesthetic technique was assessed. We aimed to avoid the risks of general anesthesia in a fragile, full-stomach old patient, and the risks of a pharmacological reversal of rivaroxaban’s anticoagulant effect to allow neuraxial techniques[6].
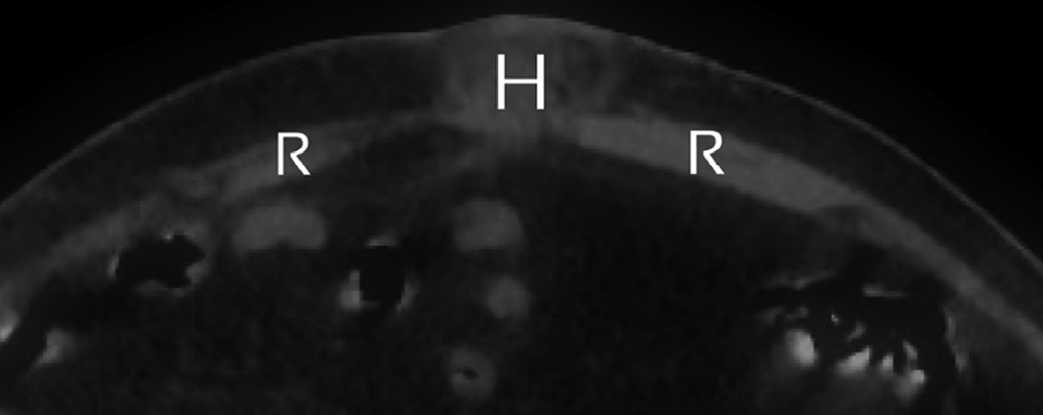
Figure 1. Original image of the abdominal CT-scan where the incarcerated umbilical hernia and rectus abdominis muscle can be identified. H: incarcerated umbilical hernia; R: rectus abdominis muscle.
For this reason, we decided to perform a bilateral RSB at the level of the umbilicus, as it was previously reported as being useful in selected cases[7],[8],[9] and it has a low bleeding risk[6]. We also performed a multimodal pain management and administered antiemetics according to the nausea and vomiting risk assessment.
As Massanero A et al., report on the first prospective study of the usefulness of RSH as an anesthetic technique, this block achieves an effective block of the muscles and parietal peritoneum, but it only gets an effective sensitive block of the skin in 53% of patients, requiring an additional local anesthetic skin infiltration9. This variable skin blockade seems to be explained by the presence of aberrant anterior cutaneous nerve branches that do not enter the posterior rectus sheath and instead perforate this muscle or travel superficially to this sheath[10]. In our case, it was not necessary to infiltrate the skin.
While RSB gets an anesthetic blockade of the abdominal wall (skin, subcutaneous tissue, muscle and parietal peritoneum), it has no influence on visceral peritoneum nor abdominal viscera[10]. Therefore, during an umbilical hernia repair, the manipulation of the gut or omentum included in the hernial sac could potentially produce discomfort, pain or vagal reflex- es. There are reports of proper clinical tolerance of these procedures under RSB and sedation. In the study carried out by Manassero A, with a sample of 30 patients for elective umbilical hernia repair without gut resection, none of the patients needed conversion to GA, and it was neither needed in our case9. It should be noted that, in case of ischemic intestinal loops requiring resection, this anesthetic technique would be insufficient and would require conversion to GA. In our case, it was necessary to resect part of the greater omentum included inside the hernial sac, but this did not produce any pain to the patient, presumably due to a low density of innervation of this fatty tissue and the sedoanalgesia achieved with remifentanil.
Postoperative recovery was faster than the usually needed after these procedures when performed under GA or spinal anesthesia, and pain management was excellent. The patient was discharged home 12 hours after the procedure without any complications.
-
Conclusions
Ultrasound-guided bilateral rectus sheath block provided anesthesia for our patient during the incarcerated umbilical hernia repair, avoiding the risks of the general and spinal anesthesia for his particular clinical situation and achieving an excellent postoperative analgesia, a fast recovery and hospital discharge without any complications.
References
1. Willschke H, Bösenberg A, Marhofer P, Johnston S, Kettner SC, Wanzel O, et al. Ultrasonography-guided rectus sheath block in paediatric anaesthesia—a new approach to an old technique. Br J Anaesth. 2006 Aug;97(2):244–9. https://doi.org/10.1093/bja/ael143 PMID:16798774
2. Ferguson S, Thomas V, Lewis I. The rectus sheath block in paediatric anaesthesia: new indications for an old technique? Paediatr Anaesth. 1996;6(6):463–6. https://doi.org/10.1046/j.1460-9592.1996.d01-24.x PMID:8936544
3. Abrahams M, Derby R, Horn JL. Update on Ultrasound for Truncal Blocks: A Review of the Evidence. Reg Anesth Pain Med. 2016;41(2):275–88. https://doi.org/10.1097/AAP.0000000000000372 PMID:26866299
4. Dolan J, Lucie P, Geary T, Smith M, Kenny GN. The rectus sheath block: accuracy of local anesthetic placement by trainee anesthesiologists using loss of resistance or ultrasound guidance. Reg Anesth Pain Med. 2009;34(3):247–50. https://doi.org/10.1097/AAP.0b013e31819a3f67 PMID:19587624
5. Robinson M, Davidson A. Aspiration under anaesthesia: risk assessment and decision-making. Contin Educ Anaesth Crit Care Pain. 2014;14(4):171–5. https://doi.org/10.1093/bjaceaccp/mkt053.
6. Vivas D, Roldán I, Ferrandis R, Marín F, Roldán V, Tello-Montoliu A, et al.; Expert reviewers. Perioperative and Periprocedural Management of Antithrombotic Therapy: consensus Document of SEC, SEDAR, SEACV, SECTCV, AEC, SECPRE, SEPD, SEGO, SEHH, SETH, SEMERGEN, SEMFYC, SEMG, SEMICYUC, SEMI, SEMES, SEPAR, SENEC, SEO, SEPA, SERVEI, SECOT and AEU. Rev Esp Cardiol (Engl Ed). 2018 Jul;71(7):553–64. https://doi.org/10.1016/j.rec.2018.01.029 PMID:29887180
7. Phua DS, Phoo JW, Koay CK. The ultrasound-guided rectus sheath block as an anaesthetic in adult paraumbilical hernia repair. Anaesth Intensive Care. 2009 May;37(3):499–500. PMID:19499877
8. Quek KH, Phua DS. Bilateral rectus sheath blocks as the single anaesthetic technique for an open infraumbilical hernia repair. Singapore Med J. 2014 Mar;55(3):e39–41. https://doi.org/10.11622/smedj.2014042 PMID:24664392
9. Manassero A, Bossolasco M, Meineri M, Ugues S, Liarou C, Bertolaccini L. Spread patterns and effectiveness for surgery after ultrasound-guided rectus sheath block in adult day-case patients scheduled for umbilical hernia repair. J Anaesthesiol Clin Pharmacol. 2015;31(3):349–53. https://doi.org/10.4103/0970-9185.161671 PMID:26330714
10. Chin KJ, McDonnell JG, Carvalho B, Sharkey A, Pawa A, Gadsden J. Essentials of Our Current Understanding: Abdominal Wall Blocks. Reg Anesth Pain Med. 2017;42(2):133–83. https://doi.org/10.1097/AAP.0000000000000545 PMID:28085788

 ORCID
ORCID


 Creative Commons Attribution
Creative Commons Attribution