Andrea Marín-Prado1, Anderson Rico-Gómez1, Eduardo Lema-Flórez1,2, Andrés Zorrilla-Vaca3, Andrés Fabricio Caballero-Lozada1, Juan Manuel Gómez-Menéndez1,2,*
Recibido: 18-08-2022
Aceptado: 22-10-2022
©2023 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 52 Núm. 3 pp. 315-319|https://doi.org/10.25237/revchilanestv5214031042
PDF|ePub|RIS
Anestesia espinal con aguja 29G punta de lápiz: experiencia unicentrica en pacientes no obstétricos
Abstract
Objectives: Spinal anesthesia is a technique in which a local anesthetic is administered into the subarachnoid space. For this, different caliber and style needles are used, one of them, the pencil point needle, has reported a lower incidence of post-dural puncture headache (PDPH) and adverse events. However, failure rates vary, possible technical difficulty being one of the causes. In this context, the objective of this study was to evalúate the incidence of PDPH, the time in seconds to obtain cerebrospinal fluid (CSF) and the anesthetic success rate with the spinal technique using a 29G pencil point needle, for non-obstetric procedures. Methods: Unique historical cohort (2016-2019) of 812 patients over 18 years old. Among the variables observed there were sociodemographic characteristics, number of lumbar puncture attempts, CSF collection time, patient position for the anesthetic procedure, type of surgery, anesthetic failure, and appearance of PDPH. Stata SE14.0 software was used for the statistical analysis of the information. Results: No cases of PDPH were observed. The average time for obtaining CSF was 86.1 seconds, with the factors associated with a higher time frame being the position in lateral decubitus and age. The anesthetic success rate was 99.2%. Conclusión: The use of the 29G pencil point needle for subarachnoid anesthesia in patients for non-obstetric surgery, in the observed cohort, reported a success rate close to 100%. The time to obtain CSF can be slow compared to the use of larger gauge needles and varies with the position and age of the patient.
Resumen
Objetivos: La anestesia espinal es una técnica en la que se administra un anestésico local en el espacio subaracnoideo. Para ello se utilizan agujas de diferentes calibres y estilos, una de ellas, la aguja de punta de lápiz ha reportado menor incidencia de cefalea post punción dural (CPPD) y eventos adversos. Sin embargo, las tasas de falla varían, siendo la posible dificultad técnica una de las causas. En este contexto, el objetivo de este estudio fue evaluar la incidencia de CPPD, el tiempo en segundos para la obtención de líquido cefalorraquídeo (LCR) y la tasa de éxito anestésico con la técnica espinal con aguja punta lápiz 29G, para procedimientos no obstétricos. Métodos: Cohorte histórica única (2016-2019) de 812 pacientes mayores de 18 años. Entre las variables observadas se encuentran las características sociodemográficas, número de intentos de punción lumbar, tiempo de recolección del LCR, posición del paciente para el procedimiento anestésico, tipo de cirugía, falla anestésica y aparición de CPPD. Para el análisis estadístico de la información se utilizó el software Stata SE14.0. Resultados: No se observaron casos de CPPD. El tiempo medio de obtención del LCR fue de 86,1 segundos, siendo los factores asociados a un mayor tiempo la posición en decúbito lateral y la edad. La tasa de éxito anestésico fue del 99,2%. Conclusiones: El uso de la aguja punta de lápiz 29G para anestesia subaracnoidea en pacientes para cirugía no obstétrica, en la cohorte observada, reportó una tasa de éxito cercana al 100%. El tiempo para obtener LCR puede ser lento en comparación con el uso de agujas de mayor calibre y varía según la posición y la edad del paciente.
-
Introduction
Spinal anesthesia, also called subarachnoid or intrathecal, is a safe neuraxial anesthetic technique used since the 19th century, which consists on the administration of local anesthetic in the subarachnoid space, with the aim of achieving a neural blockade of the fibers that transmit pain. It has a wide range of clinical applications, such as gynecological, orthopedic and general surgery surgical procedures[1].
Initially, this type of anesthesia was performed with large-caliber sharp needles (Quincke, Pitkin). In contrast, very small-caliber spinal needles with a new design called pencil point (Whitacre®, Sprotte®) are currently used. Differences in design and size improve patient safety and decrease adverse effects at the expense of effectiveness in performing the procedure due to a significant increase in the number of needle reinsertions[2], difficulties when locating the subarachnoid space and with this a possible higher incidence of anesthetic failure[3]. Studies on the use of 29G PL spinal needles are widely reported in obstetric patients[2].
A complication that has motivated the improvement of the technique and the needle used for the procedure is the presence of PDPH[4], which occurs between 0.38%-6.3% of all approaches in the neuraxis[5], but it can be as high as 25% if sharp and large caliber needles are used[6] with an impact on patient satisfaction and the need for readmissions, delayed recovery and consumption of medication for management. PL needles have a lower incidence of PDPH than sharp ones[7]. Some of the risk factors for the appearance of PDPH are age, sex, pregnancy, previous history of PDPH, orientation of the bevel at the time of the procedure, the number of lumbar puncture attempts, and the clinical experience of the operator[8]-[10].
In relation to anesthetic failure and technical difficulty of spinal anesthesia, it has been described that these are greater the smaller the caliber of the spinal needle[1],[8],[9],[11],[12]. In addition, regarding the shape of the needle tip in the literature, publications with interventions up to number 27G PL are registered, and the failure incidence is compared to the use of needles of the same caliber. An important technical aspect to consider is the time it takes to obtain CSF, which can be prolonged over 30 seconds, when 29G gauge needles are used [9]. Some of the factors that increase the time to obtain CSF are age, sex, body mass index, and position during the procedure.
The use of 29G pencil point needles has become popular in many institutions[13],[14], however, there is no evidence of publications on PDPH, recording in seconds of CSF collection time and incidence of anesthetic failure in non- obstetrics patients. Therefore, our institution decided to collect retrospective information on a historical cohort that included adult patients undergoing non-obstetric surgery under spinal anesthesia using 29G pencil point needles. We aimed to describe the characteristics of subarachnoid puncture with a 29G pencil point needle, incidence of PDPH, time to obtain CSF after puncture, and anesthetic success rate in the population.
-
Materials and Methods
A retrospective cohort study was conducted at the [Blinded], in [Blinded], between 2016 and 2019. 812 patients over 18 years that underwent non-obstetric surgery under spinal anesthesia with 29G PL needles were included. Patients scheduled for obstetric surgery and for who the neuraxial technique was contraindicated were excluded.
Full monitoring was performed in the operating room according to basic ASA standards. Sitting position was always preferred, however, in some patients lateral decubitus position was chosen because the surgical indication required a combined Spinal-Epidural technique, specifically in hip surgery where patients leaned on the non-diseased hip, spinal anesthesia with hypobaric local anesthetic was administered first and then the epidural technique was performed without the anesthesiologist being in a hurry. Patients were premedicated according to the following scheme: patients under 60 years received fentanyl 50 mcg IV + midazolam 1 mg IV, patients over 60 years only received fentanyl 50 mcg IV.
Through a medium approach, aseptic technique and antisepsis of the lumbar region was performed with chlorhexidine, after infiltration of local anesthetic in the determined area and while using a 22G x 38 mm introducer, the spinal needle 29G x 90 mm pencil point was passed through, (UNIEVER SPINAL ANESTHESIA NEEDLE (Pencil Point) Whitacre, Ref code No. 5320261, Unisis corporation, Japan) to the subarachnoid space, at which time rupture of the dura (plop) and subsequent CSF collection were noted using a chronometer. It was not possible to perform barbotage due to the high resistance of the small caliber of the needle and the possible collapse on aspiration, which could lead to mistakenly thinking that it is not in the subarachnoid space and to a failure in the anesthetic technique.
Patients were then placed in the supine position and clinical response was assessed. Sociodemographic data including age, gender, weight, and height were obtained. In addition, information was collected on the number of procedure attempts, CSF collection time (counted from the moment CSF is visualized at the beginning of the needle), patient position, type of surgery, number of attempts to reach the subarachnoid space, technique failure (if there was difficulty in reaching the space), anesthetic failure (patient requiring conversion to general anesthesia 30 minutes after the neuraxial approach) and presence of suggestive symptoms of PDPH during the first 30 postoperative days[15].
An exploratory analysis of quantitative variables was initially performed using measures of central tendency as averages (± standard deviations) or medians. Categorical variables were also represented in terms of percentages and absolute frequencies. Subsequently, a comparative analysis of the clinical and anthropometric characteristics was carried out according to the success or failure of the spinal technique using the Wilcoxon signed-rank test or Chi-square, according to the type of variable. Likewise, the characteristics were compared according to the number of puncture attempts. The Pearson correlation between these characteristics and the time of CSF collection was determined, including the patient’s position during the technique, anthropometric measurements, age and type of surgery. A P-value less than 0.05 was considered statistically significant. All analyzes were run in Stata v14.0 software (StataCorp).
This study was conducted considering the principles of the Declaration of Helsinki, and the standards of good conduct and scientific integrity, abiding by the protocols of the work center and good clinical practices on publication and the right to privacy and the informed consent. The study was approved by the institution’s Human Ethics Committee by reference CEI – 466 and act No. 240 of March 19, 2020. The anesthetic plan was explained, and the respective informed consent was obtained from all participants prior to the approach.
-
Results
In total 812 patients were included in the cohort. The mean age was 51 years. The patient’s median weight was 71 kg, with a maximum value of 118 kg and a minimum one of 40 kg. The maximum BMI value (kg/m2) was 43, with a median of 26.7. The minimum height was 1.40 m, the maximum 1.89 m and the median 1.63 m. 56% of the population was classified as ASA I, 43% ASA II and only 0.30% ASA III. Regarding the type of elective surgery performed, orthopedic surgery was the most frequent (87%), followed by General Surgery (10%) and finally Gynecological (3%). Table 1 shows the demographic and clinical variables in the population.
98% of the cases were performed on the patient in a sitting position. The average time for obtaining CSF was 86.1 seconds (min 50, max 317). Table 2 shows the statistically significant factors related to the time of CSF collection, highlighting age with a linear relationship from 70 years on (p: < 0.001 CI: 0.05 – 0.22) (Figure 1), and the lateral decubitus position (p: < 0.001 CI: 53.7 – 77.7).
No patient in the retrospective cohort presented PDPH (0%). The maximum number of attempts of the anesthetic technique was 5 (1 patient) with a median of 1 attempt (94.12%) (Figure 2). A success rate of 99.2% was obtained. Only in 6 patients there was failure in the spinal technique with the need for conversion to general anesthesia.
Table 1. Failure analysis in spinal anesthesia
| Total (n = 812) | Success (n = 806) | Failure (n =6) | |
| Age, years (average ± SD) | 50.6 ± 18.0 | 50.6 ± 17.9 | 61.3 ± 24.1 |
| Femeale, Gender (n, %) | 558 (69%) | 554 (68%) | 4 (66%) |
| Weight, kg (average ± SD) | 71 ± 12 | 70.9 ± 12.1 | 72.7 ± 8.1 |
| Height, m (average ± SD) | 1.63 ± 0.09 | 1.63 ± 0.09 | 1.59 ± 0.07 |
| Number of attempts (median, IQR) | 1 (1-1) | 1 (1-1) | 1 (1-1) |
| Time to obtain CSF seconds (average ± SD) | NA | 86.1 ± 23.5 | NA |
| Position (n, %) | |||
| Sitting | 799 (98%) | 793 (98%) | 6 (100%) |
| Lateral decubitus | 13 (2%) | 13 (2%) | 0 (0%) |
| Type of surgery (n, %) | |||
| Orthopedic | 709 (87%) | 703 (87%) | 6 (100%) |
| Gynecological | 25 (3%) | 25 (3%) | 0 (0%) |
| General surgery | 78 (10%) | 78 (10%) | 0 (0%) |
NA: Not applicable; SD: Standard deviation; CSF: Cerebrospinal fluid; IQR: Interquartile range.
Table 2. Factors related to the time to obtain CSF
| Univariate Analysis | Multivariate Regression | ||
| Value p | p coeficient | 95%CI | |
| Age | < 0.001 | +0.142 sec | 0.05 – 0.22 |
| Female, Gender | 0.0002 | +2.87 sec | -0.70 a 6.46 |
| Weight | 0.0042 | -0.112 sec | -0.25 a 0.03 |
| Size | 0.015 | -0.805 sec | -20 to 18.4 |
| Number of attempts | 0.760 | – | – |
| Position (Lateral decubitus vs sitting) | < 0.001 | +65.7 sec | 53.7 – 77.7 |
| Type of surgery (n, %) | 0.319 | – | – |
| Constant | NA | +85.2 | 54.7 to 115.7 |
NA: Not applicable; CI: Confidence interval
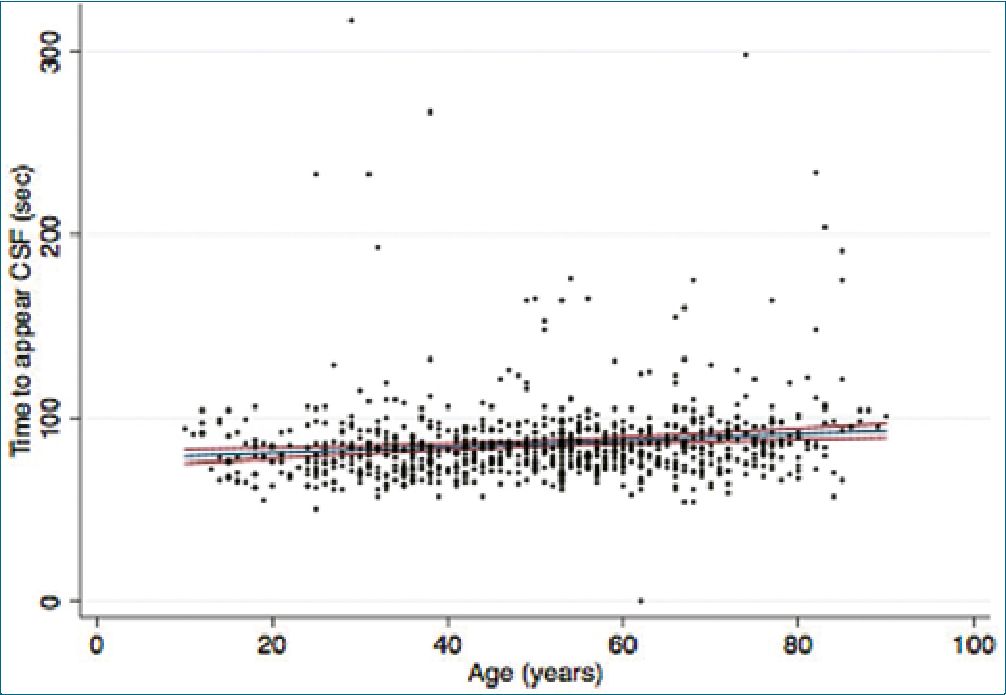
Figure 1. Patient age in relation to CSF collection time.
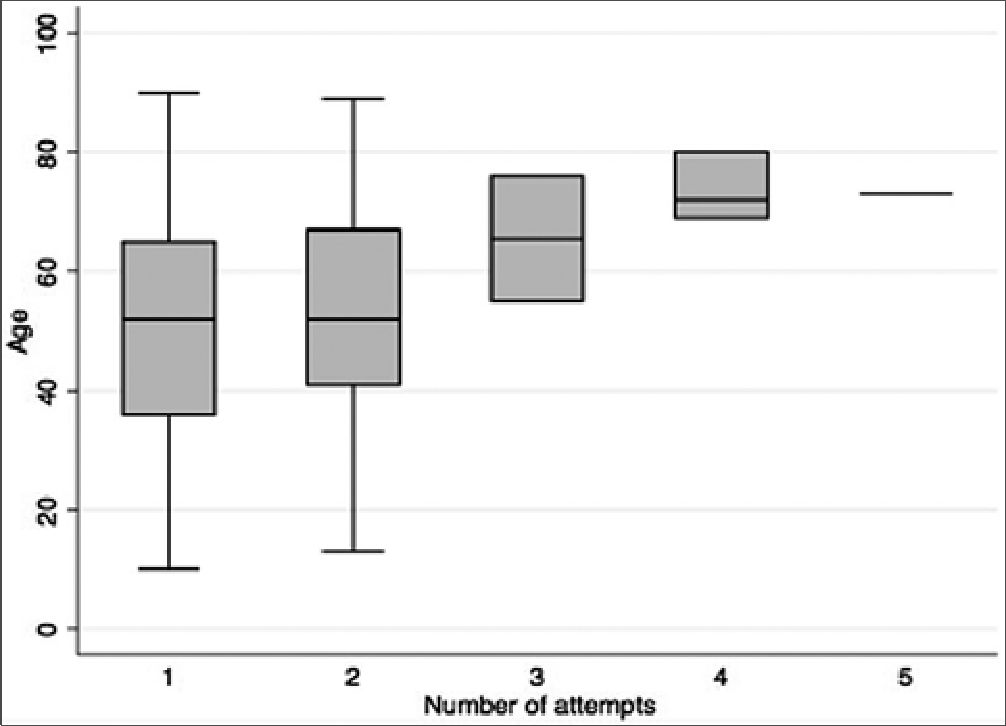
Figure 2. Age of the patient in relation to the number of lumbar puncture attempts.
-
Discussion
In the descriptive cohort of non-obstetric patients, the spinal anesthetic technique performed with a 29G PL needle does not result in any cases of PDPH, the number of attempts for the procedure is low, and the success rate is high (99.2%). It is important to recognize the prolonged CSF collection times, which reached up to 300 seconds after puncturing the arachnoid. In the multivariate analysis, two factors were found to be closely related to prolonged CSF collection time, the most relevant being age and lateral decubitus position. This feature must be taken into account by the operator because it can give the anesthesiologist the impression of a possible anesthetic failure without it actually being one. However, it should be recognized that these long CSF collection times suggest that the usefulness of this spinal needle design and caliber should be considered for patients requiring urgent surgery or for those older than 70.
Complications related to the use of subarachnoid anesthesia include a wide spectrum that ranges from insufficient conditions to perform the surgical procedure, development of transitory or permanent neurological lesions, PDPH[16], cardiovascular collapse[17], and even death[18]. The art’s current state has helped make these situations very rare in subarachnoid anesthesia. The 29G pencil point needle is, to date, the main technological development, however, in many countries its use has not been widespread yet, perhaps due to technical difficulties at the time of performing the lumbar puncture. The non-recommendation of its use in urgent surgeries and the necessary wait to obtain post-puncture CSF can be interpreted as difficulties resulting in the little use of this type of spinal needle design and caliber.
In this historical cohort study, it is observed that complications concerning the use of the 29G pencil point needle are very low. The reported success rate is 99.2%, resulting in failure of the anesthetic technique as the main complication in 6 patients (0.8%) with the need to convert to general anesthesia after 30 minutes. 3 of the complication were caused due to the impossibility of locating the subdural space, while, on the other 3, even though the subdural space was reached and the local anesthetic was applied, it was necessary to supplement the anesthesia due to insufficient blockade. In this cohort of more than 800 patients, no case of PDPH or transient or definitive neurological deficit was reported during the 30 postoperative days of the patients.
Given this panorama of results, one of the reasons why the use of the needle is not further widespread may be due to the difficulty to carry out the procedure from the technical point of view, secondary to the lack of familiarity and exposure to its use and which can be confused with technical difficulties inherent to the procedure itself. Although the time for obtaining CSF on average exceeds one minute (86.1 seconds), and may vary due to factors related to the position and conditions of the patient, this represents only one of the characteristics with which the operator must become familiar, and vary the certainty indicator of the position of the needle in the subarachnoid space of the CSF outflow towards the tactile sensation generated by the plop of the needle passing through the dural membrane and the immediate visualization of CSF in the proximal part of the needle. The usual practices that are carried out with other needle calibers such as barbotage or active CSF aspiration will not produce any results since, due to the caliber of this needle, return will not be possible.
A limitation of this work is that it is not a clinical trial, which makes it difficult to compare the results, since it is only possible to describe what was observed in the cohort. Another limitation is that the procedure and follow-up of the cohort was performed by a single anesthesiologist. We believe that more anesthesiologists should become familiar with the use of the 29G pencil point needle in order to conduct more studies and increase publications on the matter. Equally, we consider that not having assessed pain at the time of puncture, the non-measurement of patient satisfaction with the anesthetic technique suggests new studies should be carried out for the evaluation of these objectives.
Subarachnoid anesthesia has been extensively studied in the obstetric population[19],[20]. This historical cohort of patients for non-obstetric surgery describes a very high success rate with the use of the 29G pencil point needle without any reports of PDPH. The main challenge is represented by the need to become familiar with technical details such as the use of the introducer to pass the spinal needle and the importance of the plop passing of the dural membrane’s perception. Other challenges are the visualization of the proximal end of the needle with CSF as the main signs of certainty of location and the awareness required from the operator to wait for the CSF to be obtained, abolishing the aspiration or barbotage practices during the subarachnoid drug injection.
-
Conclusions
In the observed cohort of 812 non-obstetric patients, the 29G pencil point needle offers a high anesthetic success rate and no cases of PDPH, with a low number of attempts. It is important to recognize that since the time to obtain CSF can be prolonged with the use of the 29 GPL needle, its indication in urgent procedures or for those who do not tolerate the sitting position for a long time may be limited. It is also highlighted that the CSF collection time increases with age. However, it is important to recognize that our results can also be influenced by the low-risk group of patients evaluated, in which only few presented an entity of low occurrence.
Funding statement: Authors state no funding was involved.
Conflict of interest statement: The authors have disclosed no conflicts of interest.
References
1. Morros-Viñoles C, Pérez-Cuenca MD, Cedó-Lluís E, Colls C, Bueno J, Cedó-Vallobá F. [Comparison of efficacy and complications of 27G and 29G Sprottte needles for subarachnoid anesthesia]. Rev Esp Anestesiol Reanim. 2002 Nov;49(9):448–54. PMID:12516488
2. Ciftci T, Daskaya H, Efe S. Comparing spinal blockade effectiveness and maternal hemodynamics using 25 gauge and 29 gauge spinal needles with the same volumetric flow rate in patients undergoing caesarean section. J Obstet Gynaecol. 2017 Aug;37(6):719–22. https://doi.org/10.1080/01443615.2017.1290055 PMID:28375713
3. Bouchacourt V. Causas de fallas del bloqueo subaracnóideo; formas de evitarlas. Anest Analg Reanim. 2005 Aug;20(1):31–7.
4. Xu H, Liu Y, Song W, Kan S, Liu F, Zhang D, et al. Comparison of cutting and pencil-point spinal needle in spinal anesthesia regarding postdural puncture headache: A meta-analysis. Medicine (Baltimore). 2017 Apr;96(14):e6527. https://doi.org/10.1097/MD.0000000000006527 PMID:28383416
5. Haller G, Cornet J, Boldi MO, Myers C, Savoldelli G, Kern C. Risk factors for post-dural puncture headache following injury of the dural membrane: a root-cause analysis and nested case-control study. Int J Obstet Anesth. 2018 Nov;36:17–27. https://doi.org/10.1016/j.ijoa.2018.05.007 PMID:30392650
6. Geurts JW, Haanschoten MC, van Wijk RM, Kraak H, Besse TC. Post-dural puncture headache in young patients. A comparative study between the use of 0.52 mm (25-gauge) and 0.33 mm (29-gauge) spinal needles. Acta Anaesthesiol Scand. 1990 Jul;34(5):350–3. https://doi.org/10.1111/j.1399-6576.1990.tb03101.x PMID:2143882
7. Lotfy Mohammed E, El Shal SM. Efficacy of different size Quincke spinal needles in reduction of incidence of Post-Dural Puncture Headache (PDPH) in Caesarean Section (CS). Randomized controlled study. Egypt J Anaesth. 2017 May;33(1):53–8. https://doi.org/10.1016/j.egja.2016.10.011.
8. Santanen U, Rautoma P, Luurila H, Erkola O, Pere P. Comparison of 27-gauge (0.41-mm) Whitacre and Quincke spinal needles with respect to post-dural puncture headache and non-dural puncture headache. Acta Anaesthesiol Scand. 2004 Apr;48(4):474–9. https://doi.org/10.1111/j.0001-5172.2004.00345.x PMID:15025611
9. Tarkkila P, Huhtala J, Salminen U. Difficulties in spinal needle use. Insertion characteristics and failure rates associated with 25-, 27- and 29-gauge Quincke-type spinal needles. Anaesthesia. 1994 Aug;49(8):723–5. https://doi.org/10.1111/j.1365-2044.1994.tb04410.x PMID:7943709
10. Kwak K-H. Postdural puncture headache. kja 2017 Feb; 70(2): 136–143. https://doi.org/10.4097/kjae.2017.70.2.136.
11. Dittmann M, Schaefer HG, Renkl F, Greve I. Spinal anaesthesia with 29 gauge Quincke point needles and post dural puncture headache in 2,378 patients. Acta Anaesthesiol Scand. 1994 Oct;38(7):691–3. https://doi.org/10.1111/j.1399-6576.1994.tb03978.x PMID:7839778
12. Carson DF, Serpell MG. Clinical characteristics of commonly used spinal needles. Anaesthesia. 1995 Jun;50(6):523–5. https://doi.org/10.1111/j.1365-2044.1995.tb06044.x PMID:7618667
13. Sayeed YG, Sosis MB, Braverman B, et al. An in vitro investigation of the relationship between spinal needle design and failed spinal anesthetics. Reg Anesth Pain Med 1993 mar; 18(2) 18: 85.
14. Shah VR, Bhosale GP. Spinal anaesthesia in young patients: evaluation of needle gauge and design on technical problems and postdural puncture headache. South African J Anaesth Analg; 16(3). https://doi.org/10.1080/22201173.2010.10872677.
15. Arnold M. Headache classification committee of the international headache society (IHS) the international classification of headache disorders, 3rd edition. Cephalalgia 2018; 38(1): 1–211.
16. DelPizzo K, Luu T, Fields KG, Sideris A, Dong N, Edmonds C, et al. Risk of Postdural Puncture Headache in Adolescents and Adults. Anesth Analg. 2020 Jul;131(1):273–9. https://doi.org/10.1213/ANE.0000000000004691 PMID:32058449
17. Abukhouskaya N, Kowalczyk R, Górniewski G, Janiak M, Kosson D, Trzebicki J. [Hypotension – a complication of subarachnoid anesthesia especially dangerous in patients aged]. Pol Merkuriusz Lek. 2020 Jun;48(285):215–20. PMID:32564050
18. Tao KM, Sokha S, Yuan HB. The challenge of safe anesthesia in developing countries: defining the problems in a medical center in Cambodia. BMC Health Serv Res. 2020 Mar;20(1):204. https://doi.org/10.1186/s12913-020-5068-z PMID:32164745
19. Gratz I, Baruch M, Takla M, et al. The application of a neural network to predict hypotension and vasopressor requirements non-invasively in obstetric patients having spinal anesthesia for elective cesarean section (C/S). BMC Anesthesiol 2020 May; 20(1): 98: 1–15. https://doi.org/10.1186/s12871-020-01015-9.
20. Chan JJ, Tan CW, Yeam CT, Sultana R, Sia AT, Habib AS, et al. Risk Factors Associated with Development of Acute and Sub-Acute Post-Cesarean Pain: A Prospective Cohort Study. J Pain Res. 2020 Sep;13:2317–28. https://doi.org/10.2147/JPR.S257442 PMID:32982395

 ORCID
ORCID



 Creative Commons Attribution
Creative Commons Attribution