Daniel Pérez-Ajami1,*, Elisa Viscasillas Navarro2, Rasha Pérez Ajami3, Pilar Argente Navarro1, Hugo Arrando Barbera1, Luis García León1
Recibido: 29-07-2023
Aceptado: 20-08-2023
©2024 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 53 Núm. 2 pp. 189-191|https://doi.org/10.25237/revchilanestv53n2-13
PDF|ePub|RIS
Caso clínico: Perforación atrial derecha durante implante de marcapaso definitivo
Abstract
An 82-year-old male patient, who underwent permanent DDDR pacemaker implantation due to Mobitz II type AV block, attended the emergency room due to limiting dyspnoea seven days after hospital discharge. Mild hypoxemia was observed in the emergency room and he was admitted for observation and monitoring. On the ward, a regulated echocardiography was performed, revealing pericardial effusion without right chamber collapse and left pleural effusion causing complete atelectasis of the basal lobe, and a chest CT scan was scheduled to confirm the diagnosis of atrial perforation. Treatment was performed conservatively with clinical observation and drainage of both effusions, without the need to remove and reimplant the pacemaker leads.
Resumen
Un paciente varón de 82 años, al que se implantó un marcapasos permanente DDDR debido a un bloqueo AV tipo Mobitz II, acudió a urgencias por disnea limitante siete días después del alta hospitalaria. En urgencias se observó hipoxemia leve y fue ingresado para observación y monitorización. En planta se realizó una ecocardiografía reglada que reveló derrame pericárdico sin colapso de la cámara derecha y derrame pleural izquierdo con atelectasia completa del lóbulo basal, y se programó una TC torácica para confirmar el diagnóstico de perforación auricular. El tratamiento se realizó de forma conservadora con observación clínica y drenaje de ambos derrames, sin necesidad de retirar y reimplantar los cables del marcapasos.
-
Case report
The case of an 82-year-old male patient who attended the emergency room for syncopal episodes of cardiogenic characteristics with spontaneous recovery is described.
Mobitz II type second-degree atrioventricular block was diagnosed, for which a permanent DDDR pacemaker was implanted without periprocedural incidents. Seven days later, the patient went to the emergency department due to drowsiness and dyspnoea on small efforts, presenting a basal saturation of 89% and slightly decreased blood pressure. The cardiology department was admitted and a regulated transthoracic echocardiography was performed, revealing a moderate pericardial effusion without collapse of the right cavities together with a moderate
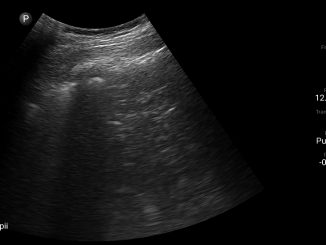
left pleural effusion (approximately 600 millilitres with an ultrasound calculation) that caused complete atelectasis of the left lower lobe (Figure 1). After these findings, it was decided to place a pleural drain and pericardiocentesis of the pericardial effusion together with close clinical surveillance and complementing the study with a chest CT scan; in which it is finally described that the distal end of the RA lead electrode is lodged in the pericardial space, surpassing the free wall of the atrium by 4 mm on its cranial slope. In addition, they detail hemopericardium that rectifies the contour of the right atrium and thickening and hyperdensity of the pericardial sheets as inflammatory changes (Figure 2). Given the hemodynamic stability and the non-increase in pericardial effusion in serial echocardiographies as in chest CT, a conservative approach was decided without surgical intervention so that the atrial perforation would fibrose and limit pleural and pericardial effusions. He was discharged from the hospital eleven days after his admission.
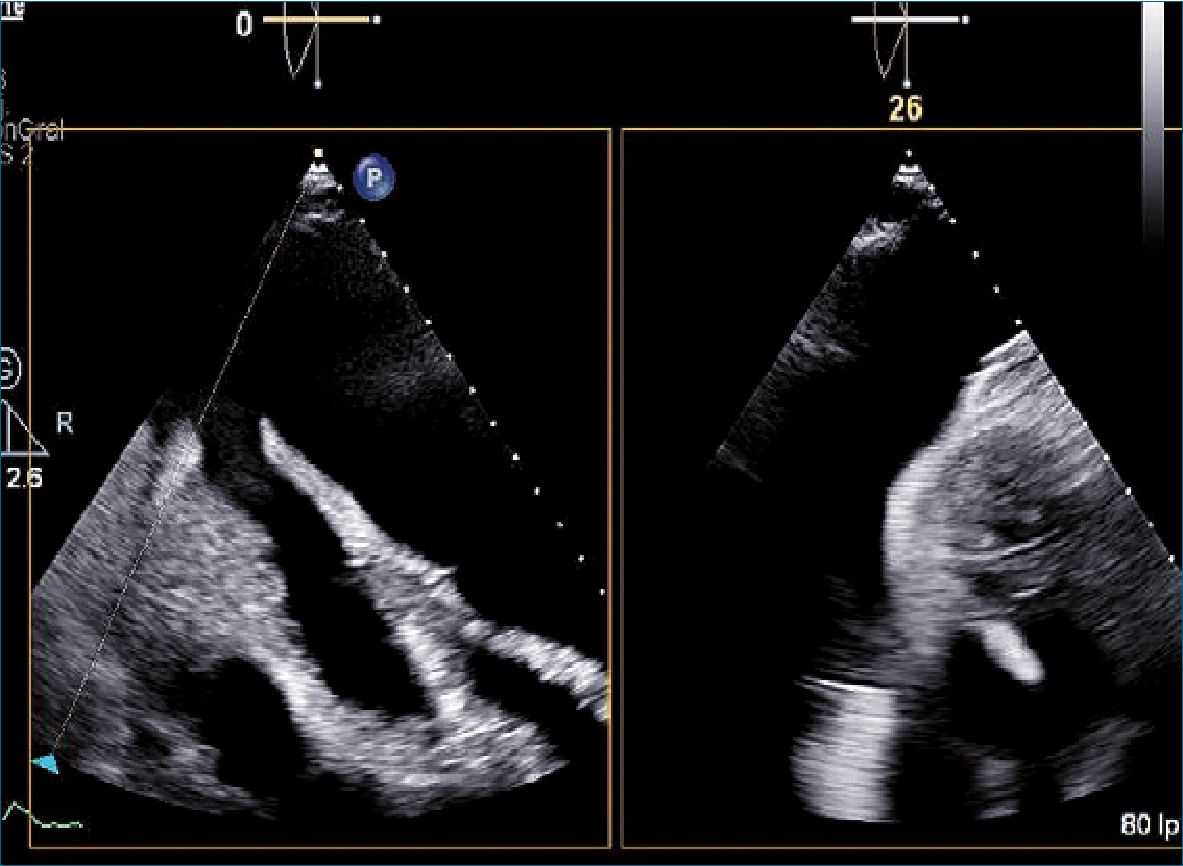
Figure 1. Echocardiography. Significant pericardial and pleural effusion with complete atelectasis of the left lower lobe.
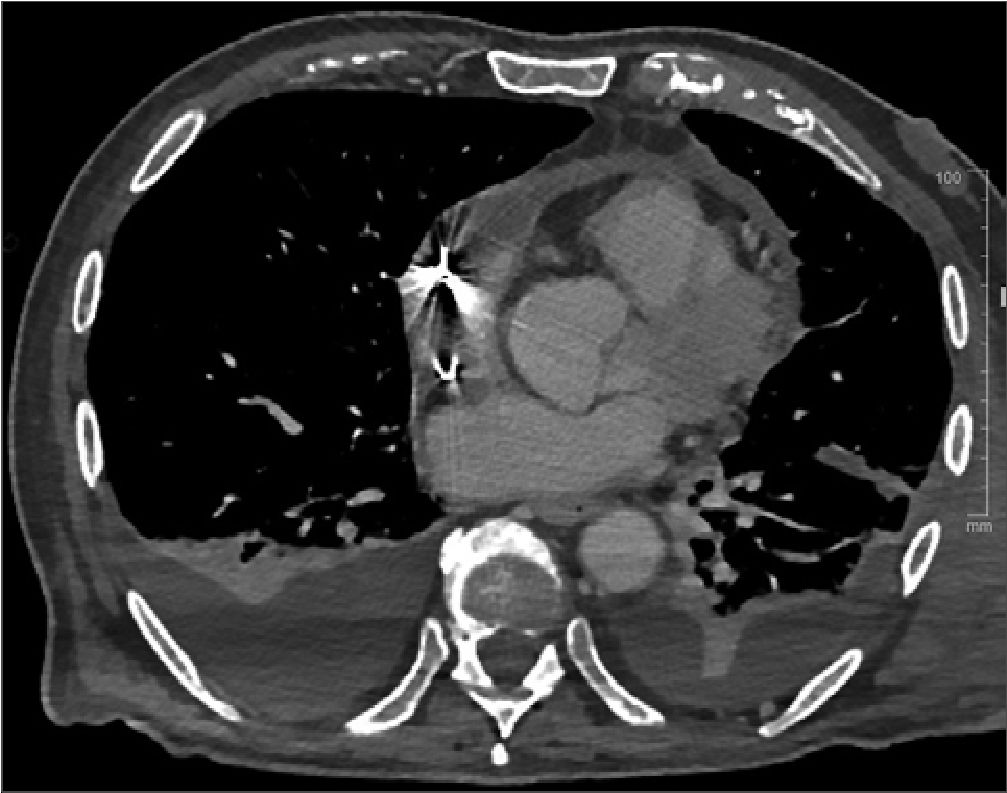
Figure 2. Chest CT. Perforation of the right atrial electrode and hemopericardium is noticed.
-
Discussion
The incidence of complications related to pacemaker implantation may vary depending on the device used and the time and place where the technique is performed. Acute complications, that is, in the first 24 hours after pacemaker implantation, occur in 3%-7% of patients, of which approximately less than 1% are due to myocardial perforation[1], the reported incidence of which is 0.5% and 0.33% for pacemakers and implantable cardioverter-defibrillators (ICDs), respectively[2].
Cardiac perforation occurs more frequently at the atrial level, being approximately twice as frequent as at the ventricular level[1]. Other complications associated with these devices can be: pneumothorax (1,5%), device displacement (2,4%), pericarditis (5%), cardiac tamponade (0,2%) and pleural effusion or hemothorax (0,1%)2, and papillary muscle rupture with valve dysfunction has even been reported. In the case of pericarditis with perforation, the risk of haemorrhagic cardiac tamponade and death may increase, so management should be stricter or follow-up should be closer in patients without
decompensated hemodynamic status[3]. The spectrum of myocardial perforation symptoms is broad, with chest pain being the most frequently documented symptom. However, up to 15% of perforations are asymptomatic, being discovered due to some subsequent complication or during routine follow-up after implantation[4].
However, there are different risk factors for presenting this complication. Cano et al.[5] described age (over 80 years), female gender, positioning of the electrode at the RV apex, and the use of drugs such as steroids as predisposing factors. The main risk factor for the patient described in this article is clearly age. At the atrial level, the main risk factor described is a wall thickness less than 2 mm[6].
Although the diagnosis may initially start from changes in the ECG that indicate a malfunction of the pacemaker, their absence does not rule out possible myocardial perforation7. Therefore, the next test to perform is a chest X-ray, which has traditionally been used to assess the position of the pacemaker electrodes in the event of suspected myocardial perforation and in which complications derived from it can also be observed such as pneumothorax or pleural effusion (Figure 3).
Transthoracic echocardiography (TTE) provides additional and fundamental information, such as the presence and amount of pericardial effusion and information on the pleural cavity, which can be affected in many clinical cases such as the one described in this text. However, it has the limitation that it usually cannot report the position of the electrode. For this reason, it is advisable to resort to other tests such as chest CT, whose spatial resolution allows the exact description of the path of the electrode and the area of myocardium involved[7].
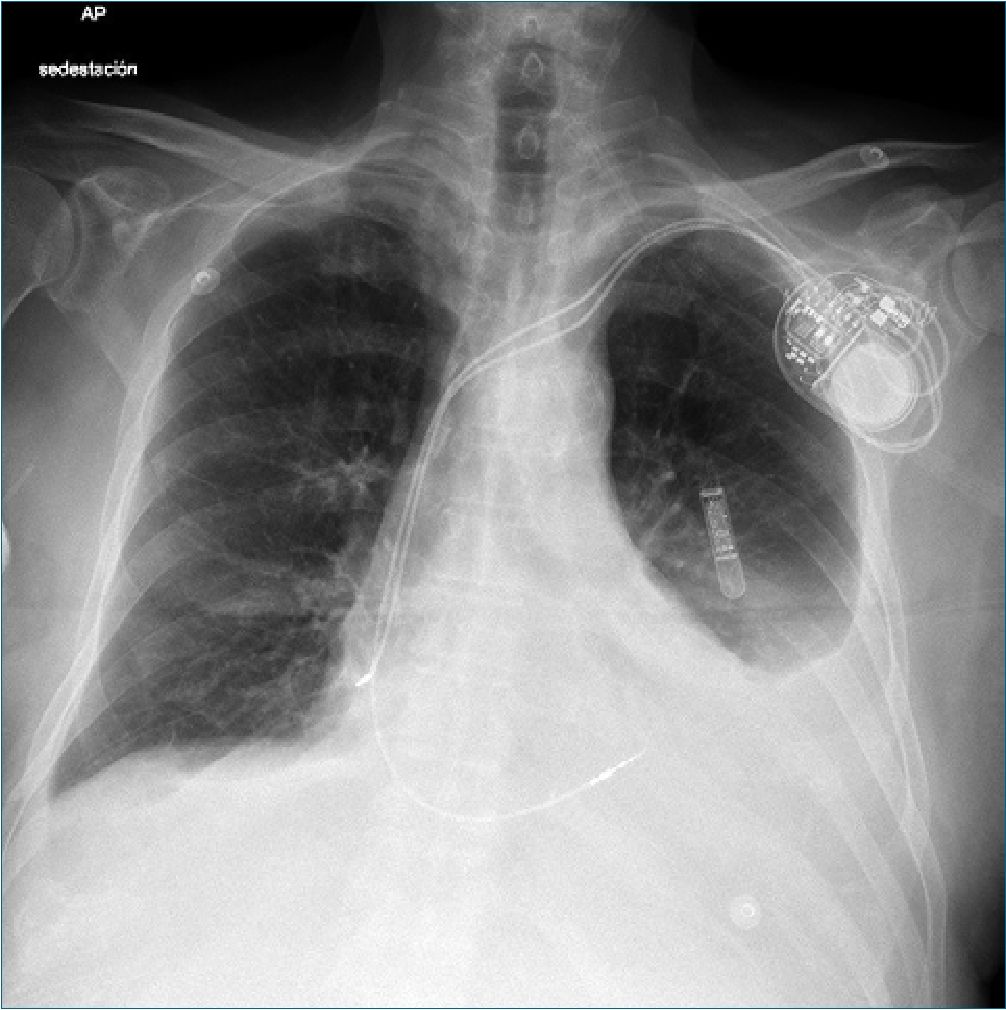
Figure 3. Cest x-ray, PA projection. Left pleural effusion is observed and the atrial electrode apparently outside the heart.
-
Conclusions
We present the clinical case of a patient with atrial perforation after placement of a permanent pacemaker, presenting clinically in an unusual manner, with hypoxemia and dyspnoea and not pericardial effusion being the main reason for consultation. This complication, despite being relatively infrequent, can be lethal, which is why a high degree of suspicion is required of the responsible physician in the face of any sign or symptom that may be a consequence of it.
Cardiac perforation is more frequent in the atrium than in the ventricle, due to the thickness of its wall, as in this case. In addition, factors such as previous temporary pacemaker implantation, active fixation electrodes, use of steroids, age over 80 years, female gender, and electrode placed in the apex of the right ventricle are associated with a higher risk of perforation. Clinically, it generally presents with retrosternal pain of moderate to severe intensity; however, we must remember that the absence of hemodynamic instability and pericardial effusion does not rule out the diagnosis of cardiac perforation, so symptoms and imaging tests are the basis of the approach of the initial suspicion of this complication. Management should be individualized for each patient. In general terms, treatment is fundamentally based on the removal and reimplantation of the lead causing the perforation, either by means of fluoroscopy or urgent cardiac surgery if the patient’s condition is critical. However, if the patient remains clinically stable, he can be treated conservatively as was the case in this case, especially in cases of atrial perforation whose wall inflammation can stabilize the perforation compared to ventricular perforation.
-
References
1. Ellenbogen KA, Wood MA, Shepard RK. Delayed complications following pacemaker implantation. Pacing Clin Electrophysiol. 2002 Aug;25(8):1155–8. https://doi.org/10.1046/j.1460-9592.2002.01155.x PMID:12358163
2. Carlson MD, Freedman RA, Levine PA. Lead perforation: incidence in registries. Pacing Clin Electrophysiol. 2008 Jan;31(1):13–5. https://doi.org/10.1111/j.1540-8159.2007.00943.x PMID:18181903
2. Tobin K, Stewart J, Westveer D, Frumin H. Acute complications of permanent pacemaker implantation: their financial implication and relation to volume and operator experience. Am J Cardiol. 2000 Mar;85(6):774–6. https://doi.org/10.1016/S0002-9149(99)00861-9 PMID:12000060
3. Hirschl DA, Jain VR, Spindola-Franco H, Gross JN, Haramati LB. Prevalence and characterization of asymptomatic pacemaker and ICD lead perforation on CT. Pacing Clin Electrophysiol. 2007 Jan;30(1):28–32. https://doi.org/10.1111/j.1540-8159.2007.00575.x PMID:17241311
4. Akbarzadeh MA, Mollazadeh R, Sefidbakht S, Shahrzad S, Bahrololoumi Bafruee N. Identification and management of right ventricular perforation using pacemaker and cardioverter-defibrillator leads: A case series and mini review. J Arrhythm. 2017 Feb;33(1):1–5. https://doi.org/10.1016/j.joa.2016.05.005 PMID:28217220
5. Cano Ó, Andrés A, Alonso P, Osca J, Sancho-Tello MJ, Olagüe J, et al. Incidence and predictors of clinically relevant cardiac perforation associated with systematic implantation of active-fixation pacing and defibrillation leads: a single-centre experience with over 3800 implanted leads. Europace. 2017 Jan;19(1):96–102. https://doi.org/10.1093/europace/euv410 PMID:26847075
6. Hao Y, Li Y, Liao D, Yang L, Liu F. A comparative analysis of the effectiveness of active versus passive atrial lead fixation in Chinese patients with cardiac implantable electrical devices: a long term, retrospective, observational, single-center study. Curr Med Res Opin. 2017 Mar;33(3):573–8. https://doi.org/10.1080/03007995.2016.1275938 PMID:28008765
7. Yavari A, Khawaja ZO, Krishnamoorthy S, McWilliams ET. Perforation of right ventricular free wall by pacemaker lead detected by multidetector computed tomography. Europace. 2009 Feb;11(2):252–4. https://doi.org/10.1093/europace/eun381 PMID:19168500

 ORCID
ORCID