Alejandro Segura O. M.D Spc. 1 ,2 , Nathali Carvajal T. M.Sc. 1 , Andrés Fabricio Caballero L. M.D Spc. 3 ,4 , Esther Cecilia Wilches L. Ph.D. 2 ,5 , Blanca Cecilia Salazar C. M.Sc. 6 ,7
Recibido: 08-04-2022
Aceptado: 06-05-2022
©2022 El(los) Autor(es) – Esta publicación es Órgano oficial de la Sociedad de Anestesiología de Chile
Revista Chilena de Anestesia Vol. 51 Núm. 5 pp. 565-571|https://doi.org/10.25237/revchilanestv5104071444
PDF|ePub|RIS
Abstract
Objective: This study aimed to determine with electrical impedance tomography (EIT) the distribution of lung volume during spontaneous breathing, between the preoperative and postoperative state of cardiac surgery. Material and Methods: This was a cross-sectional study carried out with 38 adult patients who underwent elective cardiac surgery. The distribution of global and regional pulmonary ventilation was determined through EIT, during spontaneous breathing and in a sitting position, before and after cardiac surgery. The global minute tidal variation (MTVo) and the regional minute tidal variation (MTV) were compared between these two moments, accepting p < 0.05 as a significant difference. Results: In the settings of our study, MTVdecreased without statistical significance (p = 0.74). Preoperative and postoperative regional showed substantial differences in ventilation distribution (p = 0.05), being ROI3 the most and ROI2 the least ventilated at both times. When evaluating the change from preoperative to postoperative a decrease in the left zone (ROI2 and ROI4; p = 0.049) and posterior zone (ROI3 and ROI4; p = 0.001) was observed. Conclusions: The EIT findings after cardiac surgery allowed the detection of zones of low ventilation (posterior and left) at risk for pulmonary complications.
Resumen
Objetivo: Este estudio tuvo como objetivo determinar con la tomografía de impedancia eléctrica (TIE) la distribución del volumen pulmonar durante la respiración espontánea, entre el estado preoperatorio y posoperatorio de la cirugía cardíaca. Materiales y Métodos: Se trata de un estudio transversal realizado con 38 pacientes adultos sometidos a cirugía cardíaca electiva. Se determinó la distribución de la ventilación pulmonar global y regional mediante TIE, durante la respiración espontánea y en posición sentada, antes y después de la cirugía cardíaca. Se comparó la variación tidal global por minuto (MTVo) y la variación tidal regional por minuto (MTV ROI) entre estos dos momentos, aceptando p < 0,05 como diferencia significativa. Resultados: En los escenarios de nuestro estudio, la MTVglobal disminuyó sin significación estadística (p = 0,74). Las regiones preoperatoria y posoperatoria mostraron diferencias significativas en la distribución de la ventilación (p = 0,05), siendo el ROI3 el más ventilado y el ROI2 el menos ventilado en ambos momentos. Al evaluar el cambio del preoperatorio al postoperatorio se
observó una disminución en la zona izquierda (ROI2 y ROI4; p = 0,049) y posterior (ROI3 y ROI4; p = 0,001). Conclusiones: Los hallazgos de la TIE tras la cirugía cardíaca permitieron detectar zonas de baja ventilación (posterior e izquierda) con riesgo de complicaciones pulmonares.
-
Introduction
Heart surgery by median sternotomy incision causes changes in the normal distribution of pulmonary ventilation secondary to intraoperative factors. These factors induce systemic inflammatory response syndrome, ischemia, endothelial dysfunction, pulmonary injury, and postoperative factors, such as sternotomy pain and drainage system alteration, all of which favor lung collapse[1]. The change in the distribution of ventilation can lead to postoperative pulmonary complications, with pleural effusion and atelectasis reported as being the most frequent. The onset of these complications significantly compromises lung volumes, requiring postoperative pulmonary rehabilitation to attenuate this effect[2], which is monitored by spirometry, and characterized with semiological and paraclinical evaluation[3].
Electrical impedance tomography (EIT) has recently been described as a non-invasive technique to monitor ventilation and lung perfusion without using ionizing radiation[4], which can be performed at the patient’s bedside with high temporal resolution, thus allowing real-time monitoring of the distribution of lung volume, both globally and in the regions of interest (ROI)[5]. EIT has been implemented in different studies to evaluate the distribution of ventilation among patients in the intensive care unit (ICU) with mechanical ventilatory support[6]. However, studies reporting its use in monitoring spontaneous breathing of patients after cardiac surgery are currently unknown.
The purpose of this study was to describe with EIT the distribution of lung volume during spontaneous breathing, between the preoperative and postoperative state of cardiac surgery of adult’s ICU.
-
Materials and Methods
This was an observational study with evaluation before and after cardiac surgery with 44 subjects out of 60 scheduled for open heart surgery, who were electively hospitalized from August to December 2016 in a level-III ICU in the city of Cali, Colombia.
The inclusion criteria were subjects older than 18 years, with a Body Mass Index (BMI) < 35 kg/m2, absence of pulmonary disease, confirmed by the medical examination and a normal lung function with forced expiratory volume in the first second/ forced vital capacity (FEV1/FVC) > 0.8 and FVC > 0.85, and no mental or cognitive disorders. The exclusion criteria included
hemodynamic instability manifested with insufficient perfusion with clinical features of circulatory shock or heart failure, pacemaker requirement, automatic implantable cardioverter defibrillator, incision other than median sternotomy, invasive mechanical ventilation during the postoperative period due to cardiopulmonary causes for more than 6 h, noninvasive ventilation, skin injuries or the presence of devices that prevent placement of the EIT belt.
The sociodemographic and clinical variables were obtained from clinical histories. Preoperative pulmonary status assessment included chest x-ray, simple spirometry, and the European System for Cardiac Operative Risk Evaluation rating. The total mechanical ventilation time included the hours of intraoperative ventilatory support until the time of extubation.
The project fullfilled with the principles of the Declaration of Helsinki and the Colombian scientific and technical scientific standards for health research stated in the Ministry of Health’s Resolution 8430 of 1993[7]. It was approved by the Institutional Review Board for Human Ethics of the Universidad del Valle (Minutes 012-015) and by the health institution where the study was carried out (CBI.CF-273-16). All subjects read and signed the informed consent document. The principal investigator was responsible for presenting the study to the subjects and filling out the form. A pilot test was carried out with five subjects who were not part of the sample, and adjustments were made to the protocol and the information collection forms based on the information collected.
-
EIT measurement
Lung volume distribution was evaluated before and after open-heart surgery using an electrical impedance tomograph, with the subject in a sitting position and breathing spontaneously.
The EIT was performed using a PulmoVista 500® Monitor (Drager Medical, Lübeck, Germany), to record changes in pulmonary impedance during ventilation. The PulmoVista 500® injects an alternating current through an electrode pair, and the amplitude of the resulting voltages is recorded in the other adjacent pairs to create a current profile. Current injection was rotated from electrode pair to electrode pair around the entire chest until 16 profiles with 13 measurements each were created. A total of 208 values was obtained and included in the modified Newton-Raphson algorithm by the software to reconstruct a dynamic transverse image in real time. Each EIT image was made up of a 32 x 32-pixel matrix. A low-pass filter was used at a frequency of 30 bpm to eliminate cardiac oscillations.
-
EIT and spirometry measurements
The study members and three cardiopulmonary physiotherapists with over 5 years of intensive care experience received training that included practicing the measuring technique and storing data.
A single simple spirometry measurement was performed during the preoperative visit and, if it was not inside of exclusion criteria, the subject was assessed with EIT while breathing spontaneously for 2 min. After surgery, the subject was admitted to the ICU with invasive ventilatory support, which was removed within the first 6 h after clinical and paraclinical examinations. Immediately after extubation, hemodynamic stability, pain, state of consciousness, and presence of exclusion criteria were evaluated. After 5 min, the second EIT measurement was conducted before the subject received any pulmonary re-expansion technique which consisted of sustained deep breaths and incentive spirometry[8], as part of the institutional protocol.
EIT measurements were performed with the subject in a sitting position with total back support in bed. A silicone belt with 16 electrodes was placed around the chest wall, between the 4th and 6th intercostal space, above the mid-clavicular line, just below the inter-mammary line. The sternotomy was covered during the postoperative period and the electrodes were located next to it. The thoracostomies and mediastinal drains were placed by the surgeon where they did not prevent contact with the belt. Once the equipment indicated high signal quality, the measurement was conducted and recorded on the form designed for this purpose.
To guarantee the quality of the information registered, the principal investigator conducted random reviews to confirm consistency between the original information of the tomograph, the data recorded on the forms, and the information in the database. All detected errors were corrected.
-
Functional analysis of the EIT signal
The PulmoVista 500® generated numerical values corresponding to the changes in global and regional impedance, which according to the literature, have a high correlation with the changes in ventilation R2 = 0.92[9]. The numerical value of the global minute tidal variation (MTVglobal) represents the average of the variation of the global current volume during the last minute of a record. In contrast, the numerical value of the regional minute tidal variation (MTVROI) represents the average variation of the regional current volume in the same minute [4]. The ROI analyzed were the anterior right (ROI1), anterior left (ROI2), posterior right (ROI3), and posterior left (ROI4). The zones included the sum of two regions: the anterior zone (ROI1 and ROI2), the posterior zone (ROI3 and ROI4), the right zone (ROI1 and ROI3), and the left zone (ROI2 and ROI4).
-
Statistical analysis
Analysis was performed using the IBM SPSS Statistics V22.0 statistical program. Normality of the continuous variables was determined with the Kolmogorov-Smirnov test. Variables that met the normality criteria were analyzed through average, and standard deviation and variables that did not meet them were analyzed using the median and interquartile range. Qualitative variables were evaluated through analysis of frequencies and proportions. Differences were considered significant when p < 0.05 was determined using the Student’s t-test or the Wilcoxon test in accordance with the distribution of the variables.
-
Results
Out of the 44 subjects initially included, six were excluded from the study because of a pacemaker requirement in two of them, balloon counterpulsation in one, and ventilatory support in another, leaving a sample of 38 participants. There was also one case of hemodynamic instability and one case of death. Table 1 describes the sociodemographic and preoperative clinical characteristics of the study population.
Subjects included in the study generally exhibited normal systemic function 24 h after admission to the ICU according to the sequential organ failure assessment score scale (< 4 points). Table 2 shows surgical and mechanical ventilation times, as well as the frequency of pulmonary complications, along with the regularity with which the procedures are conducted.
In the settings of our study, a non-significant decrease (p = 0.74) in MTVglobal was found in EIT ventilation distribution between before and after surgery in all study subjects (Figure 1). Figure 2 shows the MTVglobal and MTVROI of a study subject before (A) and after (B) surgery.
Preoperative and postoperative ventilation distribution was heterogeneous with significant differences in most ROIs, with greater ventilation in ROI3 and less ventilation in ROI2 at both times. A significant decrease (p = 0.05) was found only for ROIs 3 and 4 when analyzing changes in ventilation before and after surgery for each quadrant (Figure 3).
Table 1. Sociodemographic and pre-operative clinical characteristics of the population. n = 38 subjects
| Characteristic | n (%) |
| Males | 27 (71) |
| Age (years) x ± SD | 58 ± 14 |
| Pathological History | |
| Hypertension | 38 (58) |
| Tobacco use | 38 (40) |
| Diabetes | 38 (8) |
| Spirometric values * Me(IQR) | |
| FVC | 84.5 (74.7-99) |
| FEVi | 86 (72.7-99.7) |
| FEV1/FVC | 105.5 (99.7-11 1) |
| Preoperative chest x-ray | |
| Normal + | 38 (100) |
| Ejection fraction x ± SD | 60 ± 8 |
| EuroSCORE II x ± SD | 1.9 ± 1.5 |
*Median of predicted value percentages; +No evidence of pleural effusion, atelectasis, or pneumothorax; n (%) = Absolute frequency (relative frequency), Mean = x, Standard deviation = SD, Median = Me, Interquartile Range = IQR; FEV1: Forced expiratory volume in the first second; FVC: Forced vital capacity.
Table 2. Operative and postoperative characteristics of the population. n = 38 subjects
| Surgical procedures | n (%) |
| Myocardial revascularization | 12 (32) |
| Aortic valve replacement | 10 (26) |
| Mitral valve replacement | 5 (13) |
| Combined procedure (valve + revascularization) | 6 (15) |
| Bentall procedure | 2 (5) |
| Other procedures + | 3 (8) |
| Intrasurgical times (min) x ± SD | |
| Aortic clamping | 63.08 ± 32.15 |
| Extracorporeal circulation | 80.03 ± 38.53 |
| Severity scale (SOFA) (< 4) | 38 (100) |
| Total Mechanical Ventilation Time (hours) Me(IQR) | 10.5 (10-11.3) |
| Postoperative pain according to VAS x ± SD | 1.5 ± 1.8 |
| 0-1 | 24 (63) |
| 2-5 | 13 (34) |
| Postoperative chest x-ray | |
| Normal * | 33 (86.8) |
| Pulmonary complications | 5 (13.2) |
| Pleural effusion | 3 |
| Atelectasis | 1 |
| Pneumothorax | 1 |
*No evidence of pleural effusion, atelectasis and pneumothorax.
n (%) = absolute value and percentage, Mean = x, Standard deviation
= SD, Median = Me, Interquartile Range = IQR, Minutes = min.
+ One patient with myxoma and two patients with Interauricular Communication.
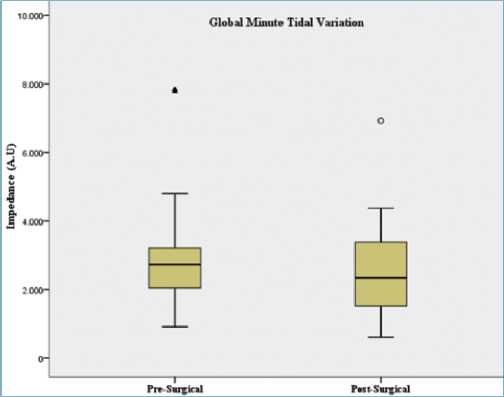
Figure 1. Global Minute Tidal Variation. Non-significant decrease (p=0,74) of Global MTV between before and after cardiac surgery in 38 patients. Extreme valúes ° and A; Y-axis: A.U: arbitrary units of impedance. X-axis: Preoperative- Postoperative.
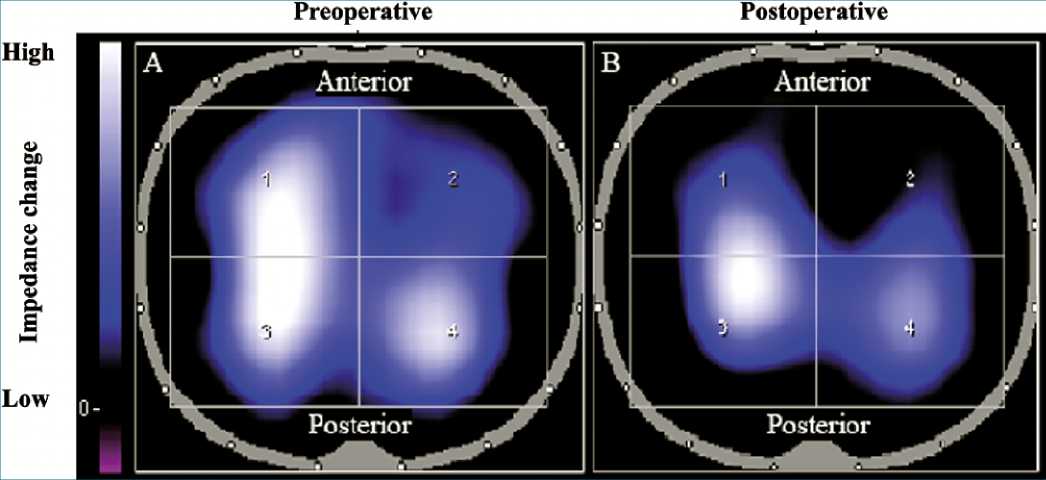
Figure 2. Image of the global and regional minute tidal variation. Images of the global and regional average minute pulmonary impedance of the same patient in the study before (A) and after (B) surgery. The areas of greater or lesser lung ventilation are represented by a chromatic scale (bar on the right) in which the dark blue color represents less ventilation, and white entails a greater ventilation. Both images were captured at the highest peak of the numerical value of the global minute tidal variation (at the end of a resting inhalation) for a period of 2 min. Y-axis: High- Impedance change- Low. X-axis: Preoperative- Postoperative. Anterior- Posterior.
When regional ventilation analysis by zone was conducted, the posterior zone (ROI3 and ROI4) showed greater ventilation than the anterior zone (ROI1 and ROI2) (p = 0.00) both under pre- and postoperative conditions. On comparing it at both moments, a significant decrease in the posterior zone (ROI3 and ROI4) was found with p = 0.001 (Figure 4). When comparing the right and left zones before surgery, it was determined that the right (ROI1 and ROI3) was significantly more ventilated than the left (ROI2 and ROI4) (p = 0.00). This difference was accentuated in the postoperative period due to the significant decrease of ventilation in the left zone (Figure 4), which also explains the difference in this zone (ROI2 and ROI4) (p = 0.049) between the pre- and postoperative condition. The pulmonary impedance values by zone are indicated in Tables 1 and 2 of the supplementary material (Figure 2).
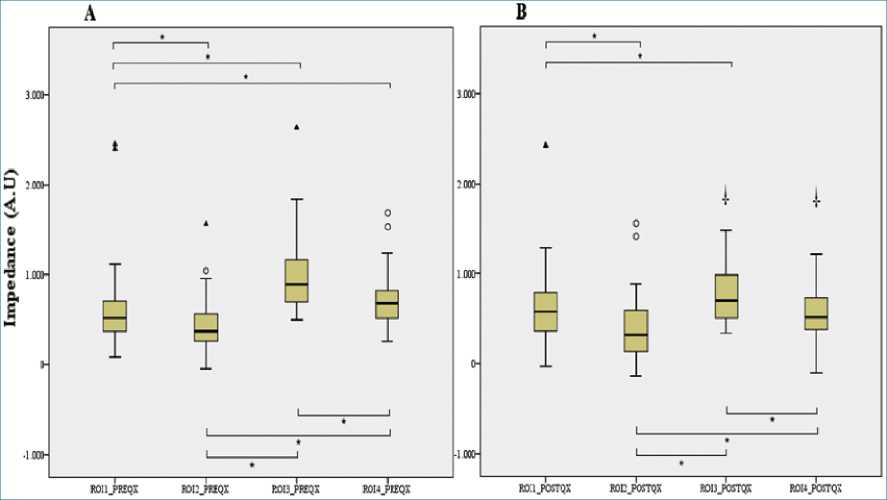
Figure 3. Pre-Surgical and Post-Surgical distribution of lung ventilation. Heterogeneity of pre-surgical ventilation distribution (A) and post-surgical ventilation distribution; (B). Extreme valúes ° and A; (A.U) arbitrary units of impedance. (*) Significant lung ventilation differences between ROIs (p < 0.05). (+) Significant differences in lung ventilation between pre-surgical and post-surgical ROIs (p < 0.005).
Figure 4. Global Minute Tidal Variation Analysis by Zones. Comparison of the right-left and anterior-posterior zones preoperative and postoperative. The impact of surgery is represented by reduced ventilation in the left and anterior zones. Extreme values ° and A; (A.U) arbitrary units of impedance. (**) Significant differences in lung ventilation between zones (p < 0.005). (+) Significant differences in lung ventilation between preoperative and postoperative zones (p < 0.05).
-
Discussion
This study represents the first report on the use of EIT in which the distribution of pulmonary ventilation in subjects undergoing cardiac surgery was analyzed before and after surgery. Lung ventilation has been traditionally assessed in this type of case by chest x-rays, arterial gases, and semiological evaluation. These forms of evaluation are mostly static, although some are invasive, and generally offer limited specific information on postoperative ventilatory changes. EIT was used in this study to analyze the distribution of pulmonary ventilation (regions and zones), considering the excellent correlation of tidal variation (in arbitrary units of impedance) with changes in lung volume, with coefficients of determination ranging from R2 = 0.92 to R2 = 0.9864[8], in spontaneous breathing.
The results obtained helped identify areas of greater postoperative ventilatory collapse, which the authors consider as a finding that will allow for the orientation of rehabilitation interventions, aimed at lowering the risk of atelectasis, reported as one of the most frequent complications of cardiac surgery, with a frequency of 16%-88%[5],[6].
Our study reported 13.2% of postoperative pulmonary complications-three subjects with small pleural effusions, one with right laminar atelectasis, and another with a lower left pneumothorax less than 15% in the presence of a thoracostomy on the same side. These findings were made upon immediate admission to the ICU and were addressed within the first 6 h, readjusting the position of the left chest tube in the subject with pneumothorax, and positioning with increased PEEP up to 8 cmH2O in the subject with atelectasis. A chest x-ray was performed to confirm the resolution of these complications before extubation. Regarding the subjects with pleural effusion, the size of this complication was considered as an insignificant impact on ventilation by the ICU team in all three cases, and conservative management was implemented. All subjects were admitted to the analysis.
A non-statistically significant decrease (p = 0.74) in the overall MTV of the subjects after cardiac surgery was found in this study (Figure 1). However, when performing the analysis by zone and region, a statistically significant decrease of the ventilation of the posterior ROI3 and ROI4 zones (p = 0.0001) and of the left ROI2 and ROI4 zones (p = 0.049) was found. The decrease in ventilation of these lung zone could be caused by the compressive effect of atmospheric pressure on the lungs after sternotomy[10], the restrictive effect of pain caused by surgical maneuvers, and the inflammatory factor of extracorporeal circulation[11].
Kraus et al. [12], assessed the change in regional pulmonary ventilation after extubation in 39 children undergoing cardiac surgery using EIT. They found a significant decrease in MTV in the ventral and dorsal areas as well, which is consistent with the effect caused by the surgery in our study. Other studies have also demonstrated the restrictive effect of cardiac surgery on the distribution of pulmonary ventilation, using different measurement techniques[3],[10], which is consistent with the findings of our research. However, the results were not reported by region in these studies.
Preoperative analysis of the distribution of pulmonary ventilation allowed us to identify ventilatory changes by region and their relationship with the risk of developing pulmonary atelectasis during the postoperative period. According to our study, preoperative EIT with spontaneous breathing showed the left anterior region (ROI2) as the least ventilated one, which continued to be less ventilated in the postoperative period, in subjects who underwent cardiac surgery. Authors believe that these findings are the result of ROI2 being the region closest to the heart[6], which has proven to be a restrictive factor for ventilation mainly because of morphological (spatial location of the heart and less left lung tissue) and gravitational (associated with the weight exerted by the heart on the left anterior area of the lung)[13]-[15] factors.
The right and posterior zones, on the other hand, had the highest ventilation (p = 0.05) both in the preoperative and postoperative periods (Figure 1). Similar results have shown these areas as having the greatest ventilation in patients evaluated in bipedal position[16] and in young and elderly patients[17].
Pulletz et al. [18], used a thoracic corset in 10 healthy men to evaluate the effect of thoracic restriction on ventilation distribution through EIT. Their main finding was associated with ventilatory descent, which, unlike in this study, was located throughout the anterior thoracic area. It is important to consider that corset restriction is only mechanical, while surgical restriction is associated with factors described above, such as the post-sternotomy compressive effect of atmospheric pressure, extracorporeal circulation inflammation, and postoperative pain. These factors reportedly not only affect certain properties of the alveolar wall, such as lung compliance or tensile activity, but also properties of the airway, such as resistance, all of which could influence the distribution of pulmonary ventilation[5],[19],[20].
The capacity to identify the areas with the highest risk of developing complications of ventilation (atelectasis) after cardiac surgery using EIT may help health professionals implement strategies that minimize risks or increase lung volume by establishing more specific and individual positioning and pulmonary re-expansion techniques.
The strengths of this study are associated with the clinical applicability of its results. To the best of our knowledge, this is the first study that analyzes cardiac patients before and after surgery and objectively evaluates changes in the pulmonary distribution of this frequent intervention. Our study proposes EIT as a tool for monitoring preventive measures and treatment of pulmonary complications after cardiac surgery as it allowed us to observe the areas at risk of developing atelectasis and provided physiological tools for the understanding of pulmonary heterogeneity.
Our study has several limitations. The authors identified the lack of studies evaluating the pre and postoperative distribution of ventilation using EIT as limitations, which made it difficult to discuss and compare the results. Furthermore, our study was based on the strong correlation (r2 > 0.92)[10],[21],[22]reported between the EIT units with units of volume (ml) and none images from recognized gold standard of lung volume as a CT- scan were taken to confirm the findings of the study. Therefore, our results were presented in arbitrary units of impedance, as reported by other studies[22]-[27]. A final limitation is that the images and information obtained from EIT Pulmovista (Drager) differs from other brands, making it difficult to compare the results with other studies that have used EIT as a tool.
Further research is required to evaluate changes in long- term pulmonary distribution after lung re-expansion exercises, which is a procedure to which these patients are usually subjected.
-
Conclusions
The EIT findings after cardiac surgery made the detection of low-ventilation zones (posterior and left) at risk for pulmonary complications.
Acknowledgements:To all the subjects who participated in the study, to the Farallones Clinic for allowing the project to be carried out in its facilities, to Draeger Colombia S.A. for allowing the use of electrical impedance tomograph as well as the physiotherapists who carried out the measurements.
Funding statement: Support Drager provided the electrical impedance tomography device that was necessary to complete this study. No financial contributions were received.
Conflict of interest statement: The authors have disclosed no conflicts of interest.
-
References
1. Ubben JF, Lance MD, Buhre WF, Schreiber JU. Clinical strategies to prevent pulmonary complications in cardiac surgery: an overview. J Cardiothorac Vasc Anesth. 2015 Apr;29(2):481–90. https://doi.org/10.1053/j.jvca.2014.09.020 PMID:25604600
2. Carsetti A, Rhodes A. How to treat post-operative complications: an evidence-based approach. Best Pract Res Clin Anaesthesiol. 2016 Jun;30(2):229–36. https://doi.org/10.1016/j.bpa.2016.04.001 PMID:27396809
3. AlOtaibi KD, El-Sobkey SB. Spirometric values and chest pain intensity three days post-operative coronary artery bypass graft surgery. J Saudi Heart Assoc. 2015 Jul;27(3):137–43. https://doi.org/10.1016/j.jsha.2015.02.002 PMID:26136627
4. Spadaro S, Mauri T, Böhm SH, Scaramuzzo G, Turrini C, Waldmann AD, et al. Variation of poorly ventilated lung units (silent spaces) measured by electrical impedance tomography to dynamically assess recruitment. Crit Care. 2018 Jan;22(1):26. https://doi.org/10.1186/s13054-017-1931-7 PMID:29386048
5. Putensen C, Hentze B, Muenster S, Muders T. Electrical Impedance Tomography for Cardio-Pulmonary Monitoring. J Clin Med. 2019 Aug;8(8):1176. https://doi.org/10.3390/jcm8081176 PMID:31394721
6. Bauer M, Opitz A, Filser J, Jansen H, Meffert RH, Germer CT, et al. Perioperative redistribution of regional ventilation and pulmonary function: a prospective observational study in two cohorts of patients at risk for postoperative pulmonary complications. BMC Anesthesiol. 2019 Jul;19(1):132. https://doi.org/10.1186/s12871-019-0805-8 PMID:31351452
7. Association WM; World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013 Nov;310(20):2191–4. https://doi.org/10.1001/jama.2013.281053 PMID:24141714
8. Alaparthi GK, Augustine AJ, Anand R, Mahale A. Comparison of Diaphragmatic Breathing Exercise, Volume and Flow Incentive Spirometry, on Diaphragm Excursion and Pulmonary Function in Patients Undergoing Laparoscopic Surgery: A Randomized Controlled Trial. Calkins CM, editor. Minim Invasive Surg. 2016 Jan;2016:1967532. https://doi.org/10.1155/2016/1967532.
9. Victorino JA, Borges JB, Okamoto VN, Matos GF, Tucci MR, Caramez MP, et al. Imbalances in regional lung ventilation: a validation study on electrical impedance tomography. Am J Respir Crit Care Med. 2004 Apr;169(7):791–800. https://doi.org/10.1164/rccm.200301-133OC PMID:14693669
10. Ragnarsdóttir M, KristjAnsdóttir A, Ingvarsdóttir I, Hannesson P, Torfason B, Cahalin L. Short-term changes in pulmonary function and respiratory movements after cardiac surgery via median sternotomy. Scand Cardiovasc J. 2004 Mar;38(1):46–52. https://doi.org/10.1080/14017430310016658 PMID:15204247
11. Baikoussis NG, Papakonstantinou NA, Verra C, Kakouris G, Chounti M, Hountis P, et al. Mechanisms of oxidative stress and myocardial protection during open-heart surgery. Ann Card Anaesth. 2015 Oct-Dec;18(4):555–64. https://doi.org/10.4103/0971-9784.166465 PMID:26440242
12. Krause U, Becker K, Hahn G, Dittmar J, Ruschewski W, Paul T. Monitoring of regional lung ventilation using electrical impedance tomography after cardiac surgery in infants and children. Pediatr Cardiol. 2014 Aug;35(6):990–7. https://doi.org/10.1007/s00246-014-0886-6 PMID:24569885
13. Riedel T, Richards T, Schibler A. The value of electrical impedance tomography in assessing the effect of body position and positive airway pressures on regional lung ventilation in spontaneously breathing subjects. Intensive Care Med. 2005 Nov;31(11):1522–8. https://doi.org/10.1007/s00134-005-2734-x PMID:16195908
14. Serrano RE, de LB, Casas O, Feixas T, Calaf N, Camacho V, et al. Use of electrical impedance tomography (EIT) for the assessment of unilateral pulmonary function. Physiol Meas. 2002 Feb;23(1):211–20. https://doi.org/10.1088/0967-3334/23/1/322 PMID:11876236
15. Frerichs I, Dudykevych T, Hinz J, Bodenstein M, Hahn G, Hellige G. Gravity effects on regional lung ventilation determined by functional EIT during parabolic flights. J Appl Physiol. 2001 Jul;91(1):39–50. https://doi.org/10.1152/jappl.2001.91.1.39 PMID:11408411
16. Ericsson E, Tesselaar E, Sjöberg F. Effect of electrode belt and body positions on regional pulmonary ventilation-and perfusion-related impedance changes measured by electric impedance tomography. PLoS One. 2016 Jun;11(6):e0155913. https://doi.org/10.1371/journal.pone.0155913 PMID:27253433
17. Frerichs I, Braun P, Dudykevych T, Hahn G, Genée D, Hellige G. Distribution of ventilation in young and elderly adults determined by electrical impedance tomography. Respir Physiol Neurobiol. 2004 Oct;143(1):63–75. https://doi.org/10.1016/j.resp.2004.07.014 PMID:15477173
18. Pulletz S, Elke G, Zick G, Schädler D, Reifferscheid F, Weiler N, et al. Effects of restricted thoracic movement on the regional distribution of ventilation. Acta Anaesthesiol Scand. 2010 Jul;54(6):751–60. https://doi.org/10.1111/j.1399-6576.2010.02233.x PMID:20397981
19. Badenes R, Lozano A, Belda FJ. Postoperative Pulmonary Dysfunction and Mechanical Ventilation in Cardiac Surgery. Annane D, editor. Crit Care Res Pract. 2015 Feb;2015:420513. https://doi.org/10.1155/2015/420513.
20. Boulpaep EL, Boron WF, Caplan MJ, Cantley L, Igarashi P, Aronson PS, et al. Medical physiology: a cellular and molecular approach. Elsevier Philadelphia (PA): Saunders; 2009.
21. Corley A, Caruana LR, Barnett AG, Tronstad O, Fraser JF. Oxygen delivery through high-flow nasal cannulae increase end-expiratory lung volume and reduce respiratory rate in post-cardiac surgical patients. Br J Anaesth. 2011 Dec;107(6):998–1004. https://doi.org/10.1093/bja/aer265 PMID:21908497
22. Spooner AJ, Corley A, Sharpe NA, Barnett AG, Caruana LR, Hammond NE, et al. Head-of-Bed Elevation Improves End-Expiratory Lung Volumes in Mechanically Ventilated Subjects: A Prospective Observational Study. Respir Care. 2014 Oct 1;59(10):1583 LP – 1589. https://doi.org/10.4187/respcare.02733.
23. Blankman P, Hasan D, Erik G, Gommers D. Detection of ‘best’ positive end-expiratory pressure derived from electrical impedance tomography parameters during a decremental positive end-expiratory pressure trial. Crit Care. 2014 May;18(3):R95. https://doi.org/10.1186/cc13866 PMID:24887391
24. Karsten J, Grusnick C, Paarmann H, Heringlake M, Heinze H. Positive end-expiratory pressure titration at bedside using electrical impedance tomography in post-operative cardiac surgery patients. Acta Anaesthesiol Scand. 2015 Jul;59(6):723–32. https://doi.org/10.1111/aas.12518 PMID:25867049
25. Reychler G, Uribe Rodriguez V, Hickmann CE, Tombal B, Laterre PF, Feyaerts A, et al. Incentive spirometry and positive expiratory pressure improve ventilation and recruitment in postoperative recovery: A randomized crossover study. Physiother Theory Pract. 2019 Mar;35(3):199–205. https://doi.org/10.1080/09593985.2018.1443185 PMID:29485340
26. Zhao Z, Steinmann D, Müller-Zivkovic D, Martin J, Frerichs I, Guttmann J, et al. A lung area estimation method for analysis of ventilation inhomogeneity based on electrical impedance tomography. J XRay Sci Technol. 2010;18(2):171–82. https://doi.org/10.3233/XST-2010-0252 PMID:20495244
27. Reifferscheid F, Elke G, Pulletz S, Gawelczyk B, Lautenschläger I, Steinfath M, et al. Regional ventilation distribution determined by electrical impedance tomography: reproducibility and effects of posture and chest plane. Respirology. 2011 Apr;16(3):523–31. https://doi.org/10.1111/j.1440-1843.2011.01929.x PMID:21261780

 ORCID
ORCID

 Creative Commons Attribution
Creative Commons Attribution